- Record: found
- Abstract: found
- Article: found
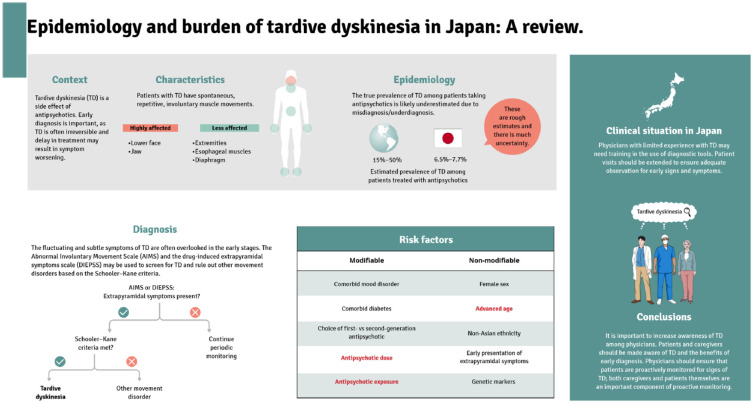
Current perspectives on the epidemiology and burden of tardive dyskinesia: a focused review of the clinical situation in Japan

Read this article at
Abstract
Tardive dyskinesia (TD) is a movement disorder that can develop with the use of dopamine receptor-blocking agents and is most commonly caused by antipsychotics. The use of antipsychotics is expanding, which may lead to an increased number of patients experiencing TD. To summarise the current knowledge of the epidemiology and risk factors for TD in Japan, we reviewed articles related to the current state of knowledge around TD identified through a PubMed search, and held a roundtable discussion of experts in Japan on 9 September 2021 to form the basis of the opinion presented within this review. The true prevalence of TD among patients treated with antipsychotics is not well characterised; it is reported to be between 15% and 50% globally and between 6.5% and 7.7% in Japan. Potential barriers to timely treatment of TD include the stigma surrounding mental health issues and the lack of data regarding TD in Asian patients. This review summarises the current knowledge of the epidemiology, challenges to TD diagnosis and risk factors for TD in Japan. Recent strategies for symptom monitoring and early diagnosis, as well as consensus recommendations are included. Achieving a high level of awareness of TD among physicians who treat patients with psychiatric disorders is of great importance and physicians should ensure that patients with psychiatric disorders receiving antipsychotics are proactively monitored for signs of TD.
Related collections
Most cited references109
- Record: found
- Abstract: found
- Article: not found
Global Epidemiology and Burden of Schizophrenia: Findings From the Global Burden of Disease Study 2016
- Record: found
- Abstract: found
- Article: not found
Adverse effects of antipsychotic medications.
- Record: found
- Abstract: found
- Article: not found