- Record: found
- Abstract: found
- Article: found
Vaccination Against Hepatitis A for Hemophilic Patients: Is It Necessary?
Read this article at
Abstract
Background
Hemophilic patients require long-life intravenous infusion of factor concentrates to treat bleedings. This could increase the risk of transmission of blood-borne infections like hepatitis C.
Objectives
The current study was aimed at investigating the immunity status against hepatitis A in hemophilic patients in south Khorasan and evaluating the necessity of hepatitis A vaccination for this population.
Patients and Methods
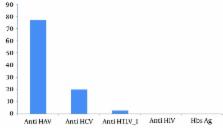
A cross-sectional descriptive study was conducted between 2014 and 2015 on all hemophilic patients of south Khorasan province, Iran (n = 108) for anti-HAV total, anti- HCV, HBs-Ag, anti-HIV, and anti-HTLV-I /II. Note that no one had already received a hepatitis A vaccine.
Results
As our results show, 77.8% of the participants (59% under 20 and 88.4% above 20 years old) were seropositive for anti-HAV total; 20.4% and 2.8% (three patients) of the cases were anti-HCV positive and anti-HTLV-1 positive, respectively, while none of the subjects were HBS-Ag or HIV-Ab positive. Seventeen of the patients (15.75%) showed a co-infection of HAV with HCV, and five HCV-infected patients (22.73%) had no immunity against hepatitis A. There was a significant relationship between age, rural life, and anti-HAV positive state in our patients (P < 0.001). No significant relationship between positive anti-HAV status and sex (P = 0.16), severity of hemophilia (P = 0.23), and infection with HIV, HCV, HTLV-1, and hepatitis B (P > 0.05) was detected.
Conclusions
More than 40% of the hemophilic patients under 20 years of age in the present study had no immunity against hepatitis A, and 23% of hepatitis C patients had not had a hepatitis A co-infection yet. Since hepatitis A can show a fulminant course in hepatitis C patients, vaccination against hepatitis A seems necessary in hemophilic patients in the region.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: not found
Hepatitis A shifting epidemiology in Latin America.
- Record: found
- Abstract: found
- Article: found