- Record: found
- Abstract: found
- Article: found
Factors associated with parametrial involvement in patients with stage IB1 cervical cancer: Who is suitable for less radical surgery?
Read this article at
Abstract
Objective
To detect the possible clinicopathologic factors associated with parametrial involvement in patients with stage IB1 cervical cancer and to identify a cohort of patients who may benefit from less radical surgery.
Methods
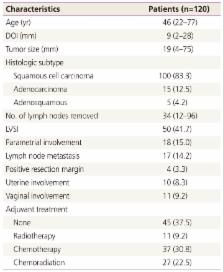
We retrospectively reviewed 120 patients who underwent radical hysterectomy and pelvic lymphadenectomy as treatment for stage IB1 cervical cancer.
Results
Overall, 18 (15.0%) patients had parametrial tumor involvement. Tumor size larger than 2 cm, invasion depth greater than 1 cm, presence of lymphovascular space involvement (LVSI), corpus involvement, and positive lymph nodes were statistically associated with parametrial involvement. Multivariate analysis for other factors showed invasion depth >1 cm ( P=0.029), and corpus involvement ( P=0.022) were significantly associated with parametrial involvement. A subgroup with tumor size smaller than 2 cm showed no parametrial involvement, regardless of invasion depth or presence of LVSI.
Conclusion
Tumor size smaller than 2 cm showed no parametrial involvement, regardless of invasion depth or presence of LVSI. Invasion depth >1 cm and corpus involvement were significantly associated with parametrial involvement in multivariate analysis. These finding may suggest that tumor size may a strong predictor of parametrial involvement in International Federation of Gynecology and Obstetrics stage IB1 cervical cancer, which can be used to select a subgroup population for less radical surgery.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Utility of parametrectomy for early stage cervical cancer treated with radical hysterectomy.
- Record: found
- Abstract: found
- Article: not found
Parametrial involvement in radical hysterectomy specimens for women with early-stage cervical cancer.
- Record: found
- Abstract: found
- Article: not found