- Record: found
- Abstract: found
- Article: found
Endoscopic Management of Peri-Pancreatic Fluid Collections
Read this article at
Abstract
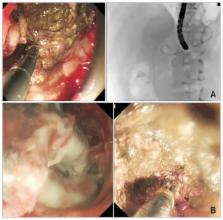
In the past decade, there has been a progressive paradigm shift in the management of peri-pancreatic fluid collections after acute pancreatitis. Refinements in the definitions of fluid collections from the updated Atlanta classification have enabled better communication amongst physicians in an effort to formulate optimal treatments. Endoscopic ultrasound (EUS)-guided drainage of pancreatic pseudocysts has emerged as the procedure of choice over surgical cystogastrostomy. The approach provides similar success rates with low complications and better quality of life compared with surgery. However, an endoscopic “step up” approach in the management of pancreatic walled-off necrosis has also been advocated. Both endoscopic and percutaneous drainage routes may be used depending on the anatomical location of the collections. New-generation large diameter EUS-specific stent systems have also recently been described. The device allows precise and effective drainage of the collections and permits endoscopic necrosectomy through the stents.
Related collections
Most cited references50
- Record: found
- Abstract: found
- Article: not found
A clinically based classification system for acute pancreatitis. Summary of the International Symposium on Acute Pancreatitis, Atlanta, Ga, September 11 through 13, 1992.
- Record: found
- Abstract: found
- Article: not found
Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos).
- Record: found
- Abstract: found
- Article: not found