- Record: found
- Abstract: found
- Article: found
Prostanoid therapies in the management of pulmonary arterial hypertension
Abstract
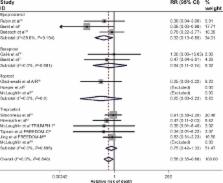
Prostacyclin is an endogenous eicosanoid produced by endothelial cells; through actions on vascular smooth-muscle cells, it promotes vasodilation. Pulmonary arterial hypertension (PAH) is characterized by elevated mean pulmonary artery pressure due to a high pulmonary vascular resistance state. A relative decrease in prostacyclin presence has been associated with PAH; this pathway has thus become a therapeutic target. Epoprostenol, the synthetic equivalent of prostacyclin, was first utilized as short-term or bridging therapy in the 1980s. Further refinement of its long-term use via continuous intravenous infusion followed. A randomized controlled trial by Barst et al in 1996 demonstrated functional, hemodynamic, and mortality benefits of epoprostenol use. This work was a groundbreaking achievement in the management of PAH and initiated a wave of research that markedly altered the dismal prognosis previously associated with PAH. Analogs of prostacyclin, including iloprost and treprostinil, exhibit increased stability and allow for an extended array of parenteral and non-parenteral (inhaled and oral) therapeutic options. This review further examines the pharmacology and clinical use of epoprostenol and its analogs in PAH.
Most cited references83
- Record: found
- Abstract: found
- Article: not found
Survival in patients with primary pulmonary hypertension. Results from a national prospective registry.
- Record: found
- Abstract: found
- Article: not found
A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension.
- Record: found
- Abstract: found
- Article: not found