- Record: found
- Abstract: found
- Article: not found
The Beck Depression Inventory (BDI-II) and a single screening question as screening tools for depressive disorder in Dutch advanced cancer patients
Read this article at
Abstract
Purpose
Depression is highly prevalent in advanced cancer patients, but the diagnosis of depressive disorder in patients with advanced cancer is difficult. Screening instruments could facilitate diagnosing depressive disorder in patients with advanced cancer. The aim of this study was to determine the validity of the Beck Depression Inventory (BDI-II) and a single screening question as screening tools for depressive disorder in advanced cancer patients.
Methods
Patients with advanced metastatic disease, visiting the outpatient palliative care department, were asked to fill out a self-questionnaire containing the Beck Depression Inventory (BDI-II) and a single screening question “Are you feeling depressed?” The mood section of the PRIME-MD was used as a gold standard.
Results
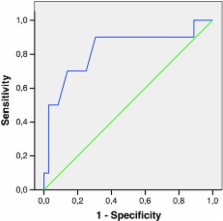
Sixty-one patients with advanced metastatic disease were eligible to be included in the study. Complete data were obtained from 46 patients. The area under the curve of the receiver operating characteristics analysis of the BDI-II was 0.82. The optimal cut-off point of the BDI-II was 16 with a sensitivity of 90% and a specificity of 69%. The single screening question showed a sensitivity of 50% and a specificity of 94%.
Related collections
Most cited references29
- Record: found
- Abstract: found
- Article: not found
On the validity of the Beck Depression Inventory. A review.
- Record: found
- Abstract: found
- Article: not found
Oncologists' recognition of depression in their patients with cancer.
- Record: found
- Abstract: found
- Article: not found
