- Record: found
- Abstract: found
- Article: found
Positive surgical margins may not affect the survival of patients with renal cell carcinoma after partial nephrectomy: A meta-analysis based on 39 studies
Read this article at
Abstract
Background
So far, whether positive surgical margin(PSM) has adverse effects on the prognosis of patients is still controversial, so we designed this study to systematically evaluate the effect of PSM on the prognosis of patients with renal cell carcinoma (RCC) after partial nephrectomy (PN).
Methods
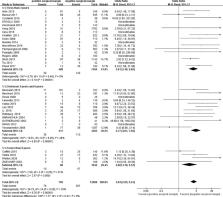
On the basis of three electronic databases (PubMed, Embase and the Cochrane Library) up to May 2022, all case–control studies (CCSs) comparing the effects of PSM and negative surgical margin (NSM) after PN on the oncological results of RCC patients were included. Two evaluators independently conducted a systematic literature search and extracted the data we needed. The methodological quality of all studies was evaluated by the modified Newcastle–Ottawa scale. The odds ratio (OR) was used to describe the results for dichotomous variables, and the meta-analysis was conducted using Cochrane Review Manager 5.2 and Stata 14.2.
Results
A total of 39 studies involving 21461 patients were included in our meta-analysis. The pooled results showed that the rates of tumor recurrence (OR 3.93, 95% CI 2.95-5.24; p < 0.00001) and metastasis (OR 4.63, 95% CI 3.11-6.88; p < 0.00001) in the PSM group were significantly higher than those in the NSM group. However, there were no significant differences in the rates of all-cause death (OR 1.35, 95% CI 0.92-1.99; p = 0.13) or cancer-specific death (OR 0.99, 95% CI 0.51-1.94; p = 0.99) between the two groups. In addition, subgroup analyses were carried out according to different average follow-ups, which revealed similar results.
Conclusion
Insignificant differences in survival between the PSM and NSM groups were observed, although significant differences in recurrence and metastasis in the PSM group were reported. Our study supported that close monitoring might be another effective choice for patients with PSM after PN. Considering the possible limitations, we recommended cautious interpretation of our results.
Related collections
Most cited references58
- Record: found
- Abstract: found
- Article: not found
Cancer Statistics, 2021

- Record: found
- Abstract: found
- Article: found
Estimating the mean and variance from the median, range, and the size of a sample
- Record: found
- Abstract: found
- Article: found