- Record: found
- Abstract: found
- Article: found
Effects of thermal environment on sleep and circadian rhythm
Read this article at
Abstract
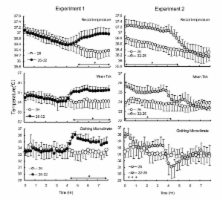
The thermal environment is one of the most important factors that can affect human sleep. The stereotypical effects of heat or cold exposure are increased wakefulness and decreased rapid eye movement sleep and slow wave sleep. These effects of the thermal environment on sleep stages are strongly linked to thermoregulation, which affects the mechanism regulating sleep. The effects on sleep stages also differ depending on the use of bedding and/or clothing. In semi-nude subjects, sleep stages are more affected by cold exposure than heat exposure. In real-life situations where bedding and clothing are used, heat exposure increases wakefulness and decreases slow wave sleep and rapid eye movement sleep. Humid heat exposure further increases thermal load during sleep and affects sleep stages and thermoregulation. On the other hand, cold exposure does not affect sleep stages, though the use of beddings and clothing during sleep is critical in supporting thermoregulation and sleep in cold exposure. However, cold exposure affects cardiac autonomic response during sleep without affecting sleep stages and subjective sensations. These results indicate that the impact of cold exposure may be greater than that of heat exposure in real-life situations; thus, further studies are warranted that consider the effect of cold exposure on sleep and other physiological parameters.
Related collections
Most cited references76
- Record: found
- Abstract: found
- Article: not found
Prognostic significance of the nocturnal decline in blood pressure in individuals with and without high 24-h blood pressure: the Ohasama study.
- Record: found
- Abstract: found
- Article: not found
Cold exposure and winter mortality from ischaemic heart disease, cerebrovascular disease, respiratory disease, and all causes in warm and cold regions of Europe. The Eurowinter Group.
- Record: found
- Abstract: found
- Article: not found