- Record: found
- Abstract: found
- Article: found
Pseudocirrhosis in Chronic Budd Chiari Syndrome With Janus Tyrosine Kinase 2 (JAK2) Mutation
case-report

23 July 2020
July 2020
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
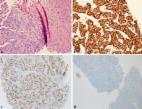
Budd-Chiari syndrome (BCS) occurs when there is hepatic venous outflow obstruction. Chronic BCS may result in liver cirrhosis due to long-standing obstruction and tend to present late. We present the first case of BCS secondary to Janus tyrosine kinase 2 (JAK2) mutation resulting in "pseudocirrhosis" rather than cirrhosis of the liver. Pseudocirrhosis clinically and radiologically mimics cirrhosis without the classical histopathological changes, and it is usually associated with metastatic cancers.
Related collections
Most cited references6
- Record: found
- Abstract: found
- Article: not found
Incidence of the JAK2 V617F mutation among patients with splanchnic or cerebral venous thrombosis and without overt chronic myeloproliferative disorders.
E. Rossi, G Leone, P. Chiusolo … (2007)
- Record: found
- Abstract: found
- Article: not found
The changing scene of hepatic vein thrombosis: recognition of asymptomatic cases.
Antoine Hadengue, Marc Poliquin, Valérie Vilgrain … (1994)
- Record: found
- Abstract: found
- Article: found
Pseudocirrhosis: A Case Series and Literature Review
Abimbola Adike, Nina Karlin, Christine O Menias … (2016)