- Record: found
- Abstract: found
- Article: found
Assessment of Hypertension Control Among Adults Participating in a Mobile Technology Blood Pressure Self-management Program
Read this article at
Key Points
Question
Is engagement with a mobile technology blood pressure self-management program associated with long-term blood pressure control?
Findings
In this cohort study of 28 189 US adults with elevated blood pressure or hypertension participating in a hypertension self-management program with a blood pressure monitor and connected smartphone application with clinically based digital coaching, most participants achieved and maintained lower blood pressure during a follow-up period that lasted as long as 3 years.
Abstract
This cohort study examines whether engagement with a hypertension self-management program with a blood pressure monitor and connected smartphone application was associated with blood pressure control among US adults.
Abstract
Importance
It is unclear whether mobile technology hypertension self-management programs are associated with blood pressure (BP) control.
Objective
To examine whether engagement with a hypertension self-management program with a BP monitor and connected smartphone application with clinically based digital coaching was associated with BP control during a follow-up period of as long as 3 years.
Design, Setting, and Participants
This cohort study enrolled US adults with elevated BP or hypertension between January 1, 2015, and July 1, 2020. The hypertension self-management program was provided through the participant’s (or their spouse’s) employer health plan.
Main Outcomes and Measures
Systolic and diastolic BP measured by a US Food and Drug Administration–cleared BP monitor, with categories defined as normal (systolic BP, <120 mm Hg), elevated (systolic BP, 120-129 mm Hg), stage 1 hypertension (systolic BP, 130-139 mm Hg), and stage 2 hypertension (systolic BP ≥140 mm Hg). Other measures included age, gender, depression, anxiety, diabetes, high cholesterol, smoking, geographic region, area deprivation index, self-reported weight, and device-measured physical activity (steps per day).
Results
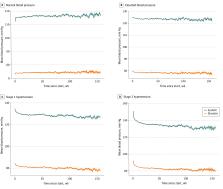
Among 28 189 participants (median [IQR] age, 51 [43-58] years; 9424 women [40.4%]; 13 902 men [59.6%]), median (IQR) baseline systolic BP was 129.5 mm Hg (120.5-139.6 mm Hg) and diastolic BP was 81.7 mm Hg (75.7-88.4 mm Hg). Median systolic BP at 1 year improved at least 1 category for 495 of 934 participants (53.0%) with baseline elevated BP, 673 of 966 (69.7%) with baseline stage 1 hypertension, and 920 of 1075 (85.7%) with baseline stage 2 hypertension. Participants in the program for 3 years had a mean (SEM) systolic BP reduction of 7.2 (0.4), 12.2 (0.7), and 20.9 (1.7) mm Hg compared with baseline for those starting with elevated, stage 1 hypertension, and stage 2 hypertension, respectively. Greater engagement was associated with lower systolic BP over time (high-engagement group: 131.2 mm Hg; 95% CI, 115.5-155.8 mm Hg; medium-engagement group: 133.4 mm Hg; 95% CI 116.3-159.5 mm Hg; low-engagement group: 135.5 mm Hg; 95% CI, 117.3-164.8 mm Hg; P < .001); these results persisted after adjusting for age, gender, depression, anxiety, diabetes, high cholesterol, smoking, area deprivation index rank, and US region, which was partially mediated by greater physical activity. A very high BP (systolic BP >180 mm Hg) was observed 11 637 times from 3778 participants. Greater engagement was associated with lower risk of very high BP; the estimated probability of a very high BP was greater in the low-engagement group (1.42%; 95% CI, 1.26%-1.59%) compared with the medium-engagement group (0.79%; 95% CI, 0.71%-0.87%; P < .001) and the high-engagement group (0.53%; 95% CI, 0.45%-0.60%; P < .001 for comparison with both groups).
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies.
- Record: found
- Abstract: found
- Article: not found
Heart Disease and Stroke Statistics—2021 Update: A Report From the American Heart Association
- Record: found
- Abstract: not found
- Article: not found