- Record: found
- Abstract: found
- Article: found
Amodiaquine-artesunate vs artemether-lumefantrine for uncomplicated malaria in Ghanaian children: a randomized efficacy and safety trial with one year follow-up
Read this article at
Abstract
Background
Artesunate-amodiaquine (AS+AQ) and artemether-lumefantrine (AM-L) are efficacious artemisinin combination therapy (ACT) regimens that have been widely adopted in sub-Saharan Africa. However, there is little information on the efficacy of these regimens on subsequent episodes beyond 28 days, or on the safety of repeated treatments.
Methods
Children aged six months to 14 years with uncomplicated malaria were randomly assigned to treatment with AS+AQ (n = 116), or AM-L (n = 111). Recruited subjects were followed-up, initially for 28 days, and then monthly for up to one year. All subsequent attacks of uncomplicated malaria after 28 days were treated with the same regimen as at randomization. Investigations aimed at determining efficacy and side effects were conducted.
Results
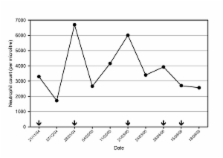
Adequate clinical and parasitological response in subjects with evaluable end-points were, 97.1% (100/103) and 98.2% (107/109) on day 14, and 94.2% (97/103) and 95.3% (102/107) on day 28 in the AM-L and AS+AQ groups, respectively. Similar results were obtained after PCR correction. The incidence of malaria attacks in the year following recruitment was similar between the two treatment groups (p = 0.93). There was a high incidence of potentially AQ-resistant parasites in the study area. The incidence of adverse events, such as pruritus, fatigue and neutropaenia were similar in the two treatment groups. No patient showed signs of hearing impairment, and no abnormal neurological signs were observed during one year of follow-up. Other adverse events were mild in intensity and overlapped with known malaria symptomatology. No adverse event exacerbation was observed in any of the subjects who received multiple treatment courses with these ACT regimens during one year follow-up.
Conclusion
AS+AQ and AM-L were efficacious for treatment of children with uncomplicated malaria in Ghana and drug-related adverse events were rare in treated subjects during one year of follow-up. The high prevalence of potentially AQ resistant parasites raises questions about the utility of AQ as a partner drug for ACT in Ghana. The efficacy of AS+AQ in Ghana requires, therefore, continuous monitoring and evaluation.
Related collections
Most cited references50
- Record: found
- Abstract: found
- Article: not found
Biased distribution of msp1 and msp2 allelic variants in Plasmodium falciparum populations in Thailand.
- Record: found
- Abstract: found
- Article: not found