- Record: found
- Abstract: found
- Article: found
Self-rated health and quality of life among Syrian refugees in Ireland – data from a cross-sectional study
Read this article at
Abstract
Introduction
As a response to the humanitarian crisis in Syria, the Irish government agreed to accept up to 4000 refugees for resettlement in Ireland in 2016. Prior to their arrival in Ireland, health screening was carried out by the International Organisation for Migration. However, no population-level measurement of the health status or needs takes place in Ireland to inform policy or health services requirements.
Methods
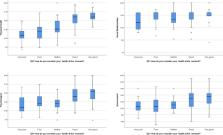
Cross-sectional data from a self-completed questionnaire among 194 Syrian Refugees aged 16 years and older resident in reception centres in Ireland in 2017/2018 is reported upon. The questionnaire measured self-reported health including quality of life and all study material were available in English and Arabic. The data was examined applying descriptive statistics and regression analysis.
Results
Syrian Refugees in Ireland consist of a relatively young cohort; in this study the majority of participants were younger than 35 years (69.5%). Two-thirds of the respondents reported their overall health status to be good or very good. The most common health condition was found to be headache and the most common medications used were painkillers. Chronic pain was experienced by one quarter of respondents; 27.5% were considered as suffering from anxiety and 10.0% had symptoms compatible with post-traumatic stress disorder (PTSD). A significant relationship was observed between chronic pain and self-rated health, as well as between chronic pain and anxiety. Quality of life (QoL) scores were lowest for the QoL environment domain.
Conclusions
Chronic pain is relatively widespread among these young and otherwise healthy refugees. Psychological distress and trauma are important factors in respondents’ quality of life scores. Chronic pain is associated with one’s mental health. Our findings and the literature suggests that the diagnosis and treatment of pain and providing care in a culturally sensitive manner should be a priority and included in the preparation and training of the relevant care providers. Additionally, the impact of living conditions on quality of life should not be underestimated.
Related collections
Most cited references21
- Record: found
- Abstract: found
- Article: not found
Understanding the co-occurrence of anxiety disorders and chronic pain: state-of-the-art.

- Record: found
- Abstract: found
- Article: found
Global patterns of mortality in international migrants: a systematic review and meta-analysis
- Record: found
- Abstract: found
- Article: not found