- Record: found
- Abstract: found
- Article: found
Predictive factors of difficulty in lower third molar extraction: A prospective cohort study
Read this article at
Abstract
Background
Several publications have measured the difficulty of third molar removal, trying to establish the main risk factors, however several important preoperative and intraoperative variables are overlooked.
Material and Methods
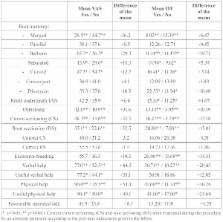
A prospective cohort study comprising a total of 130 consecutive lower third molar extractions was performed. The outcome variables used to measure the difficulty of the extraction were operation time and a 100mm visual analogue scale filled by the surgeon at the end of the surgical procedure. The predictors were divided into 4 different groups (demographic, anatomic, radiographic and operative variables). A descriptive, bivariate and multivariate analysis of the data was performed.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
The radiological prediction of inferior alveolar nerve injury during third molar surgery.
- Record: found
- Abstract: found
- Article: not found
Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction.
- Record: found
- Abstract: found
- Article: not found