- Record: found
- Abstract: found
- Article: found
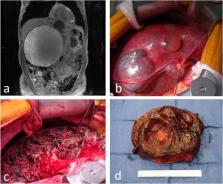
Contemporary Management of Hepatic Cyst Disease: Techniques and Outcomes at a Tertiary Hepatobiliary Center
Read this article at
Abstract
Background
Hepatic cyst disease is often asymptomatic, but treatment is warranted if patients experience symptoms. We describe our management approach to these patients and review the technical nuances of the laparoscopic approach.
Methods
Medical records were reviewed for operative management of hepatic cysts from 2012 to 2019 at a single, tertiary academic medical center.
Results
Fifty-three patients (39 female) met the inclusion criteria with median age at presentation of 65 years. Fifty cases (94.3%) were performed laparoscopically. Fourteen patients carried diagnosis of polycystic liver disease. Dominant cyst diameter was median 129 mm and located within the right lobe (30), left lobe (17), caudate (2), or was bilobar (4). Pre-operative concern for biliary cystadenoma/cystadenocarcinoma existed for 7 patients. Operative techniques included fenestration (40), fenestration with decapitation (7), decapitation alone (3), and excision (2). Partial hepatectomy was performed in conjunction with fenestration/decapitation for 15 cases: right sided (7), left sided (7), and central (1). One formal left hepatectomy was performed in a polycystic liver disease patient. Final pathology yielded simple cyst (52) and one biliary cystadenoma. Post-operative complications included bile leak (2), perihepatic fluid collection (1), pleural effusion (1), and ascites (1). At median 7.1-month follow-up, complete resolution of symptoms occurred for 34/49 patients (69.4%) who had symptoms preoperatively. Reintervention for cyst recurrence occurred for 5 cases (9.4%).
Related collections
Most cited references35
- Record: found
- Abstract: found
- Article: not found
Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey.
- Record: found
- Abstract: not found
- Article: not found
Cystic neoplasms of the liver: biliary cystadenoma and cystadenocarcinoma.
- Record: found
- Abstract: found
- Article: not found