- Record: found
- Abstract: found
- Article: found
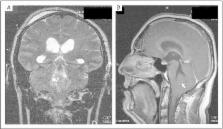
Adult Medulloblastoma Associated with Syringomyelia: A Case Report
case-report
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
The association between cerebellar medulloblastoma and syringomyelia is uncommon and only found in pediatric patients. To date, adult medulloblastoma associated with syringomyelia has not been reported in the literature. Paroxysmal bradycardia is an uncommon clinical manifestation in posterior fossa tumors and likely to be vagally mediated via brainstem preganglionic cardiac motor neurons. This report introduces the diagnosis and treatment of a case of adult medulloblastoma associated with syringomyelia, which presented with paroxysmal bradycardia.
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
Metastasis stage, adjuvant treatment, and residual tumor are prognostic factors for medulloblastoma in children: conclusions from the Children's Cancer Group 921 randomized phase III study.
P Zeltzer, J Boyett, J L Finlay … (1999)
- Record: found
- Abstract: found
- Article: not found
Management of and prognosis with medulloblastoma: therapy at a crossroads.
Gilbert Vezina, Roger Packer (2008)
- Record: found
- Abstract: found
- Article: not found
Adult medulloblastoma: prognostic factors and patterns of relapse.
Peter Chan, Aaron D. Black, J-P Loeffler … (2000)