- Record: found
- Abstract: found
- Article: found
Risk Factors for Major Early Adverse Events Related to Cardiac Catheterization in Children and Young Adults With Pulmonary Hypertension: An Analysis of Data From the IMPACT (Improving Adult and Congenital Treatment) Registry
Read this article at
Abstract
Background
Cardiac catheterization is the gold standard for assessment and follow‐up of patients with pulmonary hypertension ( PH). To date, there are limited data about the factors that influence the risk of catastrophic adverse events after catheterization in this population.
Methods and Results
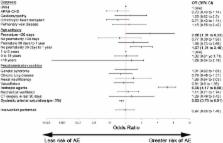
A retrospective multicenter cohort study was performed to measure risk of catastrophic adverse outcomes after catheterization in children and young adults with PH and identify risk factors for these outcomes. All catheterizations in children and young adults, aged 0 to 21 years, with PH at hospitals submitting data to the IMPACT (Improving Adult and Congenital Treatment) registry between January 1, 2011, and December 31, 2015, were studied. Using mixed‐effects multivariable regression, we assessed the association between prespecified subject‐, procedure‐, and center‐level covariates and the risk of death, cardiac arrest, or mechanical circulatory support during or after cardiac catheterization. A total of 8111 procedures performed in 7729 subjects at 77 centers were studied. The observed risk of the composite outcome was 1.4%, and the risk of death before discharge was 5.2%. Catheterization in prematurely born neonates and nonpremature infants was associated with increased risk of catastrophic adverse event, as was precatheterization treatment with inotropes and lower systemic arterial saturation. Secondary analyses demonstrated the following: (1) increasing volumes of catheterization in patients with PH were associated with reduced risk of composite outcome (odds ratio, 0.8 per 10 procedures; P=0.002) and (2) increasing pulmonary vascular resistance and pulmonary artery pressures were associated with increased risk ( P<0.0001 for both).
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
The National Cardiovascular Data Registry (NCDR) Data Quality Brief: the NCDR Data Quality Program in 2012.
- Record: found
- Abstract: found
- Article: not found
Pediatric pulmonary hypertension in the Netherlands: epidemiology and characterization during the period 1991 to 2005.
- Record: found
- Abstract: found
- Article: not found