- Record: found
- Abstract: found
- Article: found
Surgical techniques in the management of supratentorial pediatric brain tumors: 10 years’ experience at a tertiary care center in the Middle East
Read this article at
Abstract
Background:
The goal of this retrospective study is to present the first epidemiological data on pediatric supratentorial central nervous system (CNS) tumors in Lebanon and to review the various surgical management strategies used.
Methods:
We conducted a retrospective case series of all pediatric patients who presented with a supratentorial CNS tumor and underwent surgery at our institution between 2006 and 2016. We collected and analyzed demographic characteristics, tumor location, clinical manifestations, histopathology, and surgical management strategies and outcome, and discussed them after dividing the tumors as per location and in view of published literature.
Results:
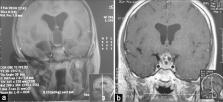
Ninety-nine children were studied with a male-to-female ratio of 2.3:1 and a mean age of 8.5 years. The most common location was convexity (44%) and included low-grade and high-grade glial tumors, along with other miscellaneous lesions. The next location was sellar/diencephalic (34%), including craniopharyngiomas, hypothalamic/optic pathway/thalamic gliomas, hamartomas, and pituitary/Rathke’s cyst, where there was notable use of endoscopic techniques (21%). Tumors in the pineal region (13%) were tectal gliomas, germ cell tumors, and pineoblastomas and were mostly treated endoscopically. The last group was lateral intraventricular tumors (8%) and was mostly choroid plexus lesions and ependymomas. Overall, the surgical objective was achieved in 95% with mild/moderate complications in 17%.
Conclusion:
A variety of pathologies may affect the pediatric population in the supratentorial region. Different surgical strategies, including microsurgical and endoscopic techniques, may be employed to remove, debulk, or biopsy these tumors depending on their location, suspected diagnosis, prognosis, and the need for treatment of possible associated hydrocephalus.
Related collections
Most cited references67
- Record: found
- Abstract: found
- Article: not found
The 2007 WHO Classification of Tumours of the Central Nervous System
- Record: found
- Abstract: not found
- Article: not found
CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2009-2013.
- Record: found
- Abstract: found
- Article: not found