- Record: found
- Abstract: found
- Article: found
Combination of Stem Cell Mobilized by Granulocyte-Colony Stimulating Factor and Human Umbilical Cord Matrix Stem Cell: Therapy of Traumatic Brain Injury in Rats
Read this article at
Abstract
Objective(s)
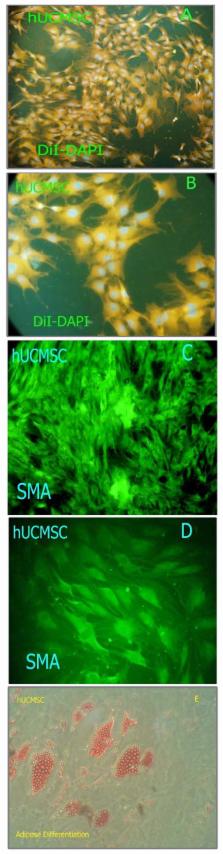
Clinical studies of treating traumatic brain injury (TBI) with autologous adult stem cells led us to examine the impression of a combination therapy. This was performed by intravenous injection of human umbilical cord matrix stem cell (hUCMSC-Wharton ,s jelly stem cell) with bone marrow cell mobilized by granulocytecolony stimulating factor (G-CSF) in rats injured with cortical compact device.
Materials and Methods
Adult male Wistar rats (n= 50) were injured with controlled cortical impact device and divided into five groups. All injections were performed 1 day after injury into the tail veins of rats. Neurological functional evaluation of animals was performed before and after injury using modified neurological severity scores (mNSS). Animals were sacrificed 42 days after TBI and brain sections were stained by Brdu immunohistochemistry.
Results
Statistically significant improvement in functional outcome was observed in treatment groups when compared with control ( P< 0.01). mNSS showed no significant differences among the hUCMSC and G-CSF treated groups at any time point (end of trial). Rats with hUCMSC + G-CSF treatment had a significant improvement on mNSS at 5 and 6 week compared to other treatment group ( P< 0.01).
Related collections
Most cited references32
- Record: found
- Abstract: found
- Article: not found
Bone marrow as a potential source of hepatic oval cells.
- Record: found
- Abstract: found
- Article: not found
A controlled cortical impact model of traumatic brain injury in the rat.
- Record: found
- Abstract: found
- Article: not found