- Record: found
- Abstract: found
- Article: not found
Continuous Glucose Monitoring: A Brief Review for Primary Care Practitioners
Read this article at
Abstract
Abstract
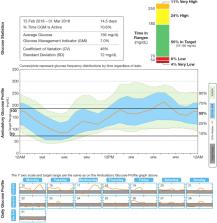
Glycated hemoglobin A1c (HbA1c) is routinely used as a marker of average glycemic control, but it fails to provide data on hypoglycemia and glycemic variability, both of which are associated with adverse clinical outcomes. Self-monitoring of blood glucose (SMBG), particularly in insulin-treated patients, is a cornerstone in the management of patients with diabetes. SMBG helps with treatment decisions that aim to reduce high glucose levels while avoiding hypoglycemia and limiting glucose variability. However, repeated SMBG can be inconvenient to patients and difficult to maintain in the long term. By contrast, continuous glucose monitoring (CGM) provides a convenient, comprehensive assessment of blood glucose levels, allowing the identification of high and low glucose levels, in addition to evaluating glycemic variability. CGM using newer detection and visualization systems can overcome many of the limitations of an HbA1c-based approach while addressing the inconvenience and fragmented glucose data associated with SMBG. When used together with HbA1c monitoring, CGM provides complementary information on glucose levels, thus facilitating the optimization of diabetes therapy while reducing the fear and risk of hypoglycemia. Here we review the capabilities and benefits of CGM, including cost-effectiveness data, and discuss the potential limitations of this glucose-monitoring strategy for the management of patients with diabetes.
Related collections
Most cited references79
- Record: found
- Abstract: found
- Article: not found
Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D Exchange clinic registry.
- Record: found
- Abstract: found
- Article: not found
Flash Glucose-Sensing Technology as a Replacement for Blood Glucose Monitoring for the Management of Insulin-Treated Type 2 Diabetes: a Multicenter, Open-Label Randomized Controlled Trial
- Record: found
- Abstract: found
- Article: not found
