- Record: found
- Abstract: found
- Article: found
Bariatric Surgery in Adolescents: To Do or Not to Do?
Read this article at
Abstract
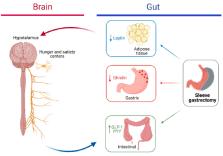
Pediatric obesity is a multifaceted disease that can impact physical and mental health. It is a complex condition that interweaves biological, developmental, environmental, behavioral, and genetic factors. In most cases lifestyle and behavioral modification as well as medical treatment led to poor short-term weight reduction and long-term failure. Thus, bariatric surgery should be considered in adolescents with moderate to severe obesity who have previously participated in lifestyle interventions with unsuccessful outcomes. In particular, laparoscopic sleeve gastrectomy is considered the most commonly performed bariatric surgery worldwide. The procedure is safe and feasible. The efficacy of this weight loss surgical procedure has been demonstrated in pediatric age. Nevertheless, there are barriers at the patient, provider, and health system levels, to be removed. First and foremost, more efforts must be made to prevent decline in nutritional status that is frequent after bariatric surgery, and to avoid inadequate weight loss and weight regain, ensuring successful long-term treatment and allowing healthy growth. In this narrative review, we considered the rationale behind surgical treatment options, outcomes, and clinical indications in adolescents with severe obesity, focusing on LSG, nutritional management, and resolution of metabolic comorbidities.
Related collections
Most cited references163
- Record: found
- Abstract: found
- Article: not found
Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents
- Record: found
- Abstract: found
- Article: found
Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity : Extended international BMI cut-offs
- Record: found
- Abstract: not found
- Article: not found