- Record: found
- Abstract: found
- Article: found
Associations Between β-Peripapillary Atrophy and Reticular Pseudodrusen in Early Age-Related Macular Degeneration
Read this article at
Abstract
Purpose
Choroidal thinning has been associated with reticular pseudodrusen (RPD) and β-peripapillary atrophy (β-PPA), which have been linked to normal-tension glaucoma (NTG). This analysis sought to determine whether RPD are independently associated with β-PPA in early AMD patients. Secondary outcomes included the association of RPD and preexisting diagnosis of glaucoma, cup-to-disc ratio (CDR), subfoveal choroidal thickness (SFCT), and IOP.
Methods
This prospective cross-sectional study examined 78 age- and sex-matched early AMD patients: 43 RPD patients (63 eyes) and 35 non-RPD patients (64 eyes). Exclusion criteria included advanced AMD, high myopia, and vitreoretinal conditions/surgery. RPD and non-RPD groups were identified by confocal scanning laser ophthalmoscopy. β-PPA as well as CDR were graded on digital, nonstereoscopic fundus photos. SFCT was measured on spectral-domain optical coherence tomography for 69 patients (35 RPD and 34 non-RPD). IOP and glaucoma diagnosis were extracted from charts.
Results
β-PPA had a greater prevalence in RPD than non-RPD (44% vs. 19%, P = 0.002); however, this relationship was not significant when SFCT was added to the model ( P = 0.150). A preexisting diagnosis of glaucoma ( P = 0.156), CDR ( P = 0.176), and IOP ( P = 0.98) was not different between groups.
Conclusions
RPD in early AMD are associated with presence of β-PPA, but choroidal thickness is a confounder in this relationship. Because β-PPA is a common finding in NTG, focusing on a potential shared pathway between RPD and NTG could improve the understanding of pathophysiology and expand therapies for each condition.
Related collections
Most cited references44
- Record: found
- Abstract: found
- Article: not found
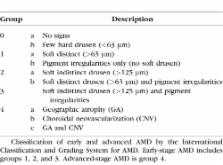
An international classification and grading system for age-related maculopathy and age-related macular degeneration. The International ARM Epidemiological Study Group.
- Record: found
- Abstract: found
- Article: not found
Prevalence of age-related maculopathy. The Beaver Dam Eye Study.
- Record: found
- Abstract: found
- Article: not found