- Record: found
- Abstract: found
- Article: found
Skeletal muscle atrogene expression and insulin resistance in a rat model of polytrauma
Read this article at
Abstract
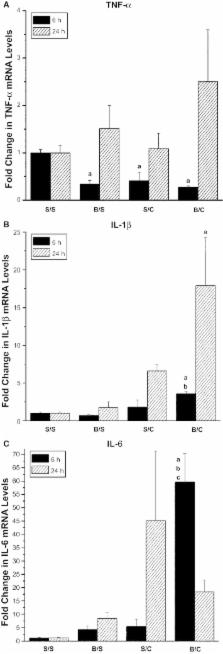
Polytrauma is a combination of injuries to more than one body part or organ system. Polytrauma is common in warfare, and in automobile and industrial accidents. The combination of injuries can include burn, fracture, hemorrhage, and trauma to the extremities or specific organ systems. Resistance to anabolic hormones, loss of muscle mass, and metabolic dysfunction can occur following injury. To investigate the effects of combined injuries, we have developed a highly reproducible rodent model of polytrauma. This model combines burn injury, soft tissue trauma, and penetrating injury to the gastrointestinal ( GI) tract. Adult, male Sprague–Dawley rats were anesthetized with pentobarbital and subjected to a 15–20% total body surface area scald burn, or laparotomy and a single puncture of the cecum with a G30 needle, or the combination of both injuries (polytrauma). In the current studies, the inflammatory response to polytrauma was examined in skeletal muscle. Changes in skeletal muscle mRNA levels of the proinflammatory cytokines TNF‐α, IL‐1β, and IL‐6 were observed following single injuries and polytrauma. Increased expression of the E3 ubiquitin ligases Atrogin‐1/ FBX032 and TRIM63/Mu RF‐1 were measured following injury, as was skeletal muscle insulin resistance, as evidenced by decreased insulin‐inducible insulin receptor ( IR) and AKT/PKB (Protein Kinase B) phosphorylation. Changes in the abundance of IR and insulin receptor substrate‐1 ( IRS‐1) were observed at the protein and mRNA levels. Additionally, increased TRIB3 mRNA levels were observed 24 h following polytrauma, the same time when insulin resistance was observed. This may suggest a role for TRIB3 in the development of acute insulin resistance following injury.
Related collections
Most cited references55
- Record: found
- Abstract: found
- Article: not found
Pathophysiology of polytrauma.
- Record: found
- Abstract: found
- Article: not found
TNF-alpha acts via p38 MAPK to stimulate expression of the ubiquitin ligase atrogin1/MAFbx in skeletal muscle.
- Record: found
- Abstract: found
- Article: not found