- Record: found
- Abstract: found
- Article: found
To reperfuse or not to reperfuse: a case report of Wellens’ syndrome with suspected COVID-19 infection
Read this article at
Abstract
Background
Wellens’ syndrome is known to be associated with left anterior descending artery occlusion that could lead to an extensive anterior wall myocardial infarction. Thus, emergency cardiac catheterization is needed. However, during coronavirus disease 2019 (COVID-19) pandemic, it is recommended for hemodynamically stable acute coronary syndrome patients with COVID-19 infection to be treated conservatively in an isolated hospital ward.
Case presentation
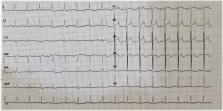
We report an 85-year-old patient with chief complaints of typical, squeezing chest pain in the past 4 h. The patient had a high fever, dyspnea, sore throat, and fatigue for 3 days. He had previously come into contact with COVID-19 positive relatives. The patient was hemodynamically stable and pulmonary auscultation revealed coarse rales in the entire lung. Electrocardiography (ECG) evaluation during the pain episode showed non-specific ST-T changes in lead V2-V5. After sublingual nitrate was administered, ECG evaluation during the pain-free period revealed a biphasic T wave inversion in lead V2 and V3. Laboratory workup showed elevated cardiac marker and leucopenia with neutrophilia and lymphopenia. Rapid immunochromatographic test and initial severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) reverse transcription-polymerase chain reaction (RT-PCR) evaluation from nasopharyngeal swab showed negative results. However, radiographic evaluations suggest the diagnosis of COVID-19 infection. While waiting for the second RT-PCR evaluation, the patient was diagnosed with Wellens’ syndrome with suspected COVID-19 infection. The patient was treated conservatively according to national guidelines and scheduled for elective cardiac catheterization. On the third day, the patient felt better and insisted on being discharged home. Ten days after discharged, the patient died of myocardial infarction.
Related collections
Most cited references6
- Record: found
- Abstract: found
- Article: not found
Cardiovascular complications in COVID-19
- Record: found
- Abstract: found
- Article: not found
Cardiovascular disease and COVID-19
- Record: found
- Abstract: found
- Article: not found