- Record: found
- Abstract: found
- Article: found
Impact of Admission Glycosylated Hemoglobin A1c on Angiographic Characteristics and Short Term Clinical Outcomes of Nondiabetic Patients with Acute ST-Segment Elevation Myocardial Infarction
Read this article at
Abstract
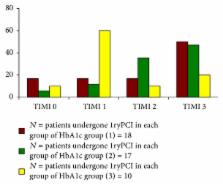
We aimed to assess the predictive value of admission HbA1c level in nondiabetic patients presented by acute STEMI, on outcome of PCI and short term outcome of adverse cardiac events. Methods. 60 nondiabetic patients were admitted to Cardiology Department, Zagazig University Hospital, with acute STMI: 27 patients with HbA1c levels of 4.5% to 6.4% (group 1), 17 patients with HbA1c levels of 6.5% to 8.5% (group 2), and 16 patients with HbA1c levels higher than 8.5% (group 3). Either invasive intervention was done at admission by (pPCI) or coronary angiography was done within month (3–28 days) from taking thrombolytic. Participants were followed up for 6 months. Results. There was significant difference among different groups of HbA1c as regards the number of diseased vessels, severity of CAD lesions ( p value < 0.01), and TIMI flow grades ( p value < 0.05). There was significant difference among different groups as regards the adverse cardiac events on short term follow-up period ( p value < 0.05). Conclusion. The present study showed that admission higher HbA1c level in patients presented by acute STEMI is associated with more severe CAD, lower rate of complete revascularization, and higher incidence of adverse cardiac events.
Related collections
Most cited references18
- Record: found
- Abstract: not found
- Article: not found
Guidelines for percutaneous transluminal coronary angioplasty. A report of the American College of Cardiology/American Heart Association Task Force on Assessment of Diagnostic and Therapeutic Cardiovascular Procedures (Subcommittee on Percutaneous Transluminal Coronary Angioplasty).
- Record: found
- Abstract: found
- Article: not found