- Record: found
- Abstract: found
- Article: found
Modulation of rabbit corneal epithelial cells fate using embryonic stem cell extract
Read this article at
Abstract
Purpose
To develop a new culture system to cultivate differentiated autologous cells in vitro for cell therapy and tissue engineering.
Methods
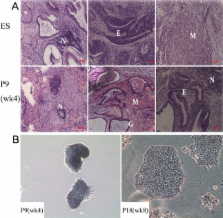
After incubation in murine embryonic stem cell (ESC) extract for 1 h, streptolysin-O (SLO) permeabilized cells were resealed with CaCl 2 and continually cultured for weeks. The morphological study was analyzed by light microscopy. Isolated colonies were selected and expanded to establish cell lines. Octamer-4 (Oct-4), stage-specific embryonic antigen-1 (SSEA-1), transformation-related protein 63 (p63), ATP-binding cassette subfamily G, member 2 (ABCG2), and cytokeratin3 (K3) were detected by indirect immunofluorescent staining. Oct-4, K3, and p63 were also detected by RT–PCR analysis. To examine the stemness characteristics of the induced cells, both alkaline phosphatase (AKP) staining and tumorigenicity detection were performed, respectively.
Results
Reprogramming was induced in corneal epithelial cells. The reprogrammed cells showed characteristics similar to ESCs in the early weeks, including colony formation, positive AKP staining, and multi-potential differentiation in vivo. Oct-4 and SSEA1 protein expression was upregulated. However, these changes were not persistent or stable. With the passage of time, the colonies became flat. The ESC markers were downregulated, while epithelial cell related proteins gradually increased.
Conclusions
Less terminal differentiated rabbit corneal epithelial cells could be induced to a more pluripotent state with embryonic stem cell extract (ESC-E). These cells have the potential to return to the beginning of their own lineage and obtain the ability of long-term growth. Our findings indicate that this culture system can generate low-immunogenic autologous cells for use in regenerative medicine.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
p63 identifies keratinocyte stem cells.
- Record: found
- Abstract: found
- Article: not found
ABCG2 transporter identifies a population of clonogenic human limbal epithelial cells.
- Record: found
- Abstract: found
- Article: not found