- Record: found
- Abstract: found
- Article: not found
Randomized Double-Blind Clinical Trial Comparing Ultra Rapid Lispro With Lispro in a Basal-Bolus Regimen in Patients With Type 2 Diabetes: PRONTO-T2D
Read this article at
Abstract
OBJECTIVE
To evaluate the efficacy and safety of ultra rapid lispro (URLi) versus lispro in patients with type 2 diabetes on a basal-bolus insulin regimen.
RESEARCH DESIGN AND METHODS
This was a phase 3, treat-to-target, double-blind 26-week study. After an 8-week lead-in to optimize basal insulin glargine or degludec in combination with prandial lispro treatment, patients were randomized to blinded URLi ( n = 336) or lispro ( n = 337) injected 0–2 min prior to meals. Patients could continue metformin and/or a sodium–glucose cotransporter 2 inhibitor. The primary end point was change in HbA 1c from baseline to 26 weeks (noninferiority margin 0.4%), with multiplicity-adjusted objectives for postprandial glucose (PPG) excursions during a standardized meal test.
RESULTS
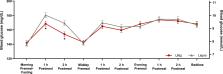
HbA 1c improved for both URLi and lispro, and noninferiority was confirmed: estimated treatment difference (ETD) 0.06% (95% CI −0.05; 0.16). Mean change in HbA 1c was −0.38% for URLi and −0.43% for lispro, with an end-of-treatment HbA 1c of 6.92% and 6.86%, respectively. URLi was superior to lispro in controlling 1- and 2-h PPG excursions: 1-h ETD, −0.66 mmol/L (95% CI −1.01, −0.30); 2-h ETD, −0.96 mmol/L (−1.41, −0.52). Significantly lower PPG excursions were evident from 0.5 to 4.0 h postmeal with URLi treatment. There were no significant treatment differences in rates of severe or documented hypoglycemia (<3.0 mmol/L). Incidence of overall treatment-emergent adverse events was similar between treatments.
Related collections
Most cited references31
- Record: found
- Abstract: found
- Article: not found
Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c).
- Record: found
- Abstract: found
- Article: not found
The treat-to-target trial: randomized addition of glargine or human NPH insulin to oral therapy of type 2 diabetic patients.
- Record: found
- Abstract: found
- Article: not found
