- Record: found
- Abstract: found
- Article: found
Impact on Visual Acuity in Neovascular Age Related Macular Degeneration (nAMD) in Europe Due to COVID-19 Pandemic Lockdown
Read this article at
Abstract
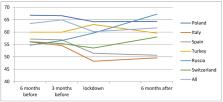
This is a retrospective, multicenter study of consecutive patients with nAMD scheduled for a visit and/or a treatment with an intravitreal injection (IVI) during the 3 months before lockdown in the Ophthalmology Departments of six centers of Europe.The study was conducted on 546 patients, of which 55.13% were females, almost 100% of the patients were White/Caucasian race, and 71.53% of the patients presented a type 1 macular neovascularization (NVM). A total of 62.82% of patients (343 patients) that were on scheduled clinic visits and/or intravitreal injection treatment during the 3 months before the quarantine did not attend either to visit or for treatment during the lockdown. The mean number of injections during the lockdown was significantly reduced. This was followed by a significant reduction in the mean best-corrected visual acuity (BCVA) between the 3 months before the lockdown (mean BCVA of 60.68 ± 19.77 letters) and 6 months after lockdown (mean BCVA of 56.98 ± 22.59 letters). Patients with better BCVA before the lockdown and the ones showing neovascular activity were more likely to attend their scheduled visits and/or IVI treatments. The COVID-19 pandemic and the lockdown have led to a decrease in the number of IVI treatments in patients with nAMD, evidencing a significant vision loss at 6 months.
Related collections
Most cited references37
- Record: found
- Abstract: found
- Article: found
Consensus Nomenclature for Reporting Neovascular Age-Related Macular Degeneration Data
- Record: found
- Abstract: found
- Article: not found
Novel method for analyzing snellen visual acuity measurements.
- Record: found
- Abstract: found
- Article: not found