- Record: found
- Abstract: found
- Article: found
Elevated plasma myoglobin level is closely associated with type 2 diabetic kidney disease
Read this article at
Abstract
Background
Diabetic kidney disease (DKD) is the most frequent complication in patients with type 2 diabetes mellitus (T2DM). It causes a chronic and progressive decline in kidney function, and ultimately patients require renal replacement therapy. To date, an increasing number of clinical studies have been conducted to explore the potential and novel biomarkers, which can advance the diagnosis, estimate the prognosis, and optimize the therapeutic strategies at the early stage of DKD. In the current study, we sought to investigate the association of plasma myoglobin with DKD.
Methods
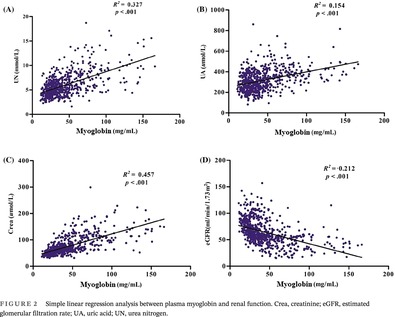
A total of 355 T2DM patients with DKD and 710 T2DM patients without DKD were enrolled in this study. Laboratory parameters including blood cell count, hemoglobin A1c, biochemical parameters, and plasma myoglobin were recorded. Patients were classified on admission according to the tertile of myoglobin and clinical parameters were compared between the groups. Pearson correlation analysis, linear regression, logistic regression, receiver operating characteristics (ROC) analysis, and spline regression were performed.
Results
Plasma myoglobin significantly increased in patients with DKD and was associated with renal function and inflammatory parameters. Plasma myoglobin was an independent risk factor for the development of DKD. The area under ROC curve of myoglobin was 0.831. Spline regression showed that there was a significant linear association between DKD incidence and a high level of plasma myoglobin when it exceeded 36.4 mg/mL.
Abstract
Related collections
Most cited references46
- Record: found
- Abstract: found
- Article: not found
WITHDRAWN: Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9th edition
- Record: found
- Abstract: found
- Article: not found
Diabetic Kidney Disease: Challenges, Progress, and Possibilities.
- Record: found
- Abstract: found
- Article: not found