- Record: found
- Abstract: found
- Article: found
Multisystem inflammatory syndrome in children during severe acute respiratory syndrome coronavirus‐2 pandemic in Turkey: A single‐centre experience
Read this article at
Abstract
Aim
Severe acute respiratory syndrome coronavirus‐2 (SARS‐CoV‐2) infection may result in a life‐threatening hyperinflammatory condition named multisystem inflammatory syndrome in children (MIS‐C). We aimed to assess demographics, clinical presentations, laboratory characteristics and treatment outcomes of patients with MIS‐C.
Methods
We performed a retrospective study of patients with MIS‐C managed between August 2020 and March 2021 at Dr. Sami Ulus Maternity Child Health and Diseases Training and Research Hospital in Turkey.
Results
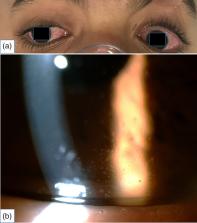
A total of 45 patients (23 male, 51%) with a median age of 8.7 years (interquartile range: 5.6–11.7 years) were enrolled to study. The SARS‐CoV‐2 serology was positive in 43 (95%) patients. Organ‐system involvement included the dermatologic in 41 (91%), cardiovascular in 39 (87%), hematologic in 36 (80%) and gastrointestinal in 36 (80%) patients. Acute anterior uveitis was diagnosed in nine (20%) patients. Two patients presented with clinical findings of deep neck infection such as fever, neck pain, trismus, swelling and induration on the cervical lymph node. One patient presented with Henoch–Schonlein purpura‐like eruption. Coronary artery dilatation was detected in five (11%) patients. For treatment of MIS‐C, intravenous immunoglobulin was used in 44 (98%) patients, methylprednisolone in 27 (60%) and anakinra in 9 (20%) patients. The median duration of hospitalisation was nine days. All patients recovered.
Conclusions
Children with MIS‐C might have variable clinical presentations. Acute anterior uveitis might be a prominent presentation of MIS‐C and require ophthalmological examination. It is essential to make patient‐based decisions and apply a stepwise approach for the treatment of this life‐threatening disease.
Related collections
Most cited references23
- Record: found
- Abstract: found
- Article: not found
Multisystem Inflammatory Syndrome in U.S. Children and Adolescents
- Record: found
- Abstract: found
- Article: not found
Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals From the American Heart Association
- Record: found
- Abstract: found
- Article: not found
