- Record: found
- Abstract: found
- Article: found
Adherence to Advisory Committee on Immunization Practices in diabetes mellitus patients in Saudi Arabia: A multicenter retrospective study

Read this article at
Abstract
BACKGROUND
Patients with diabetes mellitus (DM) are predisposed to an increased risk of infection signifying the importance of vaccination to protect against its potentially severe complications. The Centers for Disease Control and Prevention/Advisory Committee on Immunization Practices (CDC/ACIP) issued immunization re-commendations to protect this patient population.
AIM
To assess the adherence of patients with DM to the CDC/ACIP immunization recommendations in Saudi Arabia and to identify the factors associated with the vaccine adherence rate.
METHODS
An observational retrospective study conducted in 2023 was used to collect data on the vaccination records from 13 diabetes care centers in Saudi Arabia with 1000 eligible patients in phase I with data collected through chart review and 709 patients in phase II through online survey.
RESULTS
Among participants, 10.01% ( n = 71) had never received any vaccine, while 85.89% ( n = 609) received at least one dose of the coronavirus disease 2019 (COVID-19) vaccine, and 34.83% ( n = 247) had received the annual influenza vaccine. Only 2.96% ( n = 21), 2.11% ( n = 15), and 1.12% ( n = 8) received herpes zoster, tetanus, diphtheria, and pertussis (Tdap), and human papillomavirus (HPV) vaccines, respectively. For patients with DM in Saudi Arabia, the rate of vaccination for annual influenza and COVID-19 vaccines was higher compared to other vaccinations such as herpes zoster, Tdap, pneumococcal, and HPV. Factors such as vaccine recommendations provided by family physicians or specialists, site of care, income level, DM-related hospitalization history, residency site, hemoglobin A1c (HbA1c) level, and health sector type can significantly influence the vaccination rate in patients with DM. Among non-vaccinated patients with DM, the most reported barriers were lack of knowledge and fear of side effects. This signifies the need for large-scale research in this area to identify additional factors that might facilitate adherence to CDC/ACIP vaccine recommendations in patients with DM.
CONCLUSION
In Saudi Arabia, patients with DM showed higher vaccination rates for annual influenza and COVID-19 vaccines compared to other vaccinations such as herpes zoster, Tdap, pneumococcal, and HPV. Factors such as vaccine recommendations provided by family physicians or specialists, the site of care, income level, DM-related hospitalization history, residency site, HbA1c level, and health sector type can significantly influence the vaccination rate in patients with DM.
Related collections
Most cited references38
- Record: found
- Abstract: found
- Article: not found
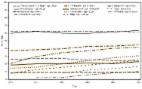
IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045

- Record: found
- Abstract: found
- Article: found
Global, regional, and national burden of diabetes from 1990 to 2021, with projections of prevalence to 2050: a systematic analysis for the Global Burden of Disease Study 2021
- Record: found
- Abstract: found
- Article: found
