- Record: found
- Abstract: found
- Article: found
Choroidal Thickness and microRNA146 in Lupus Nephritis Patients
Read this article at
Abstract
Purpose
To evaluate the choroidal thickness (CT) in the macular area in patients with lupus nephritis and to compare the results with both non-nephritic patients and normal control. To assess the relation of CT to serum microRNA146, disease duration, activity index, and medications.
Patients and Methods
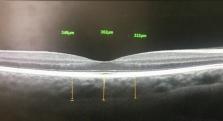
Thirty-five SLE patients and thirty normal healthy controls were enrolled for this cross-sectional prospective study. All participants have undergone optical coherence tomography using RTVue OCT (Optovue Inc., Fremont, CA, USA). The scan used was the macular cross 6-mm line. We measured CT from the posterior edge of the retinal pigment epithelium (RPE) to the choroid-sclera junction at subfovea, and 750 µm both temporal and nasal to the fovea.
Results
The mean central subfoveal CT in patients was 275.7 ± 41.0 µm (214–374 µm), and the mean central subfoveal CT in the control group was 364.5± 23.0 µm (323–411µm). There was a significant thinning at all three points in patients compared to the control group (p<0.001, Mann–Whitney U-test). In the patients group, subfoveal choroid in non-nephritic subgroup showed significant thinning compared to nephritic subgroup (p=0.032, Mann–Whitney U-test). Drusen-like deposits (DLDs) were detected in 22.9% (8/35) of patients and none in control (p=.023). MiRNA146 showed a significant positive correlation with nephritic lupus patients (r=0.036, P=0.04).
Conclusion
The choroidal thickness was significantly thicker among the nephritic lupus patients as compared to the non-nephritic subgroup. Both SLE patients’ subgroups are thinner than normal control. Subfoveal choroidal thickening can be considered a biomarker in nephritic lupus especially in conjunction with an increase in miRNA146a. All SLE patients are at risk of small Drusen-like deposits.
Related collections
Most cited references24
- Record: found
- Abstract: found
- Article: not found
A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes.
- Record: found
- Abstract: found
- Article: not found
MicroRNAs direct rapid deadenylation of mRNA.
- Record: found
- Abstract: found
- Article: not found