- Record: found
- Abstract: found
- Article: found
Severe acute interstitial nephritis secondary to minocycline use in an adolescent girl
Read this article at
Abstract
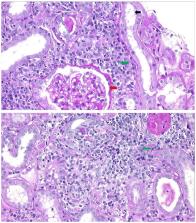
Acute interstitial nephritis is an uncommon but classic complication of minocycline therapy for acne. A 14-year-old African American girl was started on oral minocycline for the treatment of acne 6 weeks before presentation. After 4 weeks on minocycline, she developed a generalized rash, anasarca, fever, myalgia, nausea, vomiting, sore throat, and generalized body weakness. The evaluation showed increased levels of serum creatinine, urea nitrogen, and serum alanine and aspartate aminotransferases. Renal ultrasonography showed bilateral enlarged, echogenic kidneys, and percutaneous renal biopsy showed features of acute allergic interstitial nephritis. Treatment included methylprednisolone and intravenous fluids and discontinuation of minocycline. The elevated serum creatinine level (12.9 mg/dL (reference, 0.40–0.70 mg/dL)) suggests marked renal impairment corresponding with Kidney Disease Improving Global Outcomes acute kidney injury classification stage 3. The kidney injury improved from stage 3 to stage 1 within 3 days, and early treatment with steroids might have prevented chronic renal failure. The creatinine level promptly decreased to normal, and liver enzyme results also improved. In summary, the diagnosis of acute interstitial nephritis should be considered in patients who present with renal failure associated with recent use of minocycline, and treatment with corticosteroids should be considered early during the hospitalization.
Related collections
Most cited references19
- Record: found
- Abstract: found
- Article: not found
Systematic review of antibiotic resistance in acne: an increasing topical and oral threat.
- Record: found
- Abstract: not found
- Article: not found
Drug-Induced Acute Interstitial Nephritis
- Record: found
- Abstract: not found
- Article: not found