- Record: found
- Abstract: found
- Article: found
Idiopathic megacolon complicated by life-threatening giant megacolon and respiratory failure due to diaphragmatic eventration: A case report
Read this article at
Abstract
Introduction and importance
Giant megacolon requiring emergency surgery is rare. Eventration of the diaphragm associated with giant megacolon is also uncommon.
Case presentation
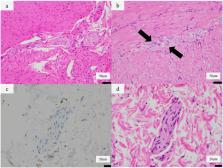
We report a 66-year-old male who presented with abdominal distention and progressive dyspnea. After resuscitation following cardiopulmonary arrest, the patient underwent emergent subtotal abdominal colectomy. Eventration of the diaphragm was found postoperatively and his respiratory condition was insufficient to allow liberation. Plication of both diaphragms was performed through left and right thoracotomy via the 8th intercostal space. Postoperatively the patient made a full recovery.
Highlights
-
•
A life-threatening condition secondary to chronic megacolon is extremely rare.
-
•
Abdominal compartment syndrome due to giant megacolon resolved by subtotal abdominal colectomy.
-
•
Chronic megacolon from childhood induced eventration of the diaphragm.
-
•
Plication of both diaphragms recovered fully the patient from respiratory dysfunction.
Related collections
Most cited references14
- Record: found
- Abstract: found
- Article: not found
The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines
- Record: found
- Abstract: found
- Article: not found
The enteric nervous system in chagasic and idiopathic megacolon.
- Record: found
- Abstract: found
- Article: not found