- Record: found
- Abstract: found
- Article: found
Critical appraisal of artificial intelligence-based prediction models for cardiovascular disease
Abstract
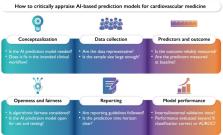
The medical field has seen a rapid increase in the development of artificial intelligence (AI)-based prediction models. With the introduction of such AI-based prediction model tools and software in cardiovascular patient care, the cardiovascular researcher and healthcare professional are challenged to understand the opportunities as well as the limitations of the AI-based predictions. In this article, we present 12 critical questions for cardiovascular health professionals to ask when confronted with an AI-based prediction model. We aim to support medical professionals to distinguish the AI-based prediction models that can add value to patient care from the AI that does not.
Graphical Abstract
Related collections
Most cited references82
- Record: found
- Abstract: found
- Article: not found
General cardiovascular risk profile for use in primary care: the Framingham Heart Study.

- Record: found
- Abstract: found
- Article: found
Prediction models for diagnosis and prognosis of covid-19 infection: systematic review and critical appraisal
- Record: found
- Abstract: found
- Article: not found
