- Record: found
- Abstract: found
- Article: found
Pre- and Postcycloplegic Refractions in Children and Adolescents
Read this article at
Abstract
Purpose
To determine the difference between cycloplegic and non-cycloplegic refractive error and its associated factors in Chinese children and adolescents with a high prevalence of myopia.
Methods
A school-based study including 1565 students aged 6 to 21 years was conducted in 2013 in Ejina, Inner Mongolia, China. Comprehensive eye examinations were performed. Pre-and postcycloplegic refractive error were measured using an auto-refractor. For cycloplegic refraction, one drop of topical 1.0% cyclopentolate was administered to each eye twice with a 5-minute interval and a third drop was administered 15 minutes after the second drop if the pupil size was less than 6 mm or if the pupillary light reflex was still present.
Results
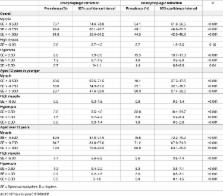
Two drops of cyclopentolate were found to be sufficient in 59% of the study participants while the other 41% need an additional drop. The prevalence of myopia was 89.5% in participants aged over 12 years and 68.6% in those aged 12 years or younger (P<0.001). When myopia was defined as spherical equivalent (SE) of less than -0.5 diopter (D), the prevalence estimates were 76.7% (95% confidence interval [CI] 74.6–78.8) and 54.1% (95%CI 51.6–56.6) before and after cycloplegic refraction, respectively. When hyperopia was defined as SE of more than 0.5D, the prevalence was only 2.8% (95%CI 1.9–3.6) before cycloplegic refraction while it was 15.5% (95%CI 13.7–17.3) after cycloplegic refraction. Increased difference between cycloplegic and non-cycloplegic refractive error was associated with decreased intraocular pressures (P = 0.01).
Conclusions
Lack of cycloplegia in refractive error measurement was associated with significant misclassifications in both myopia and hyperopia among Chinese children and adolescents. Decreased intraocular pressure was related to a greater difference between cycloplegic and non-cycloplegic refractive error.
Related collections
Most cited references18
- Record: found
- Abstract: found
- Article: not found
Refractive Error Study in Children: results from Mechi Zone, Nepal.
- Record: found
- Abstract: found
- Article: not found
Necessity of cycloplegia for assessing refractive error in 12-year-old children: a population-based study.
- Record: found
- Abstract: found
- Article: not found