- Record: found
- Abstract: found
- Article: found
The Clinical Utility of DCISionRT ® on Radiation Therapy Decision Making in Patients with Ductal Carcinoma In Situ Following Breast-Conserving Surgery
Read this article at
Abstract
Background
The role of radiation therapy (RT) following breast-conserving surgery (BCS) in ductal carcinoma in situ (DCIS) remains controversial. Trials have not identified a low-risk cohort, based on clinicopathologic features, who do not benefit from RT. A biosignature (DCISionRT ®) that evaluates recurrence risk has been developed and validated. We evaluated the impact of DCISionRT on clinicians’ recommendations for adjuvant RT.
Methods
The PREDICT study is a prospective, multi-institutional, observational registry in which patients underwent DCISionRT testing. The primary endpoint was to identify the percentage of patients where testing led to a change in RT recommendations.
Results
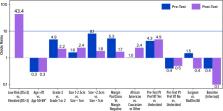
Overall, 539 women were included in this study. Pre DCISionRT testing, RT was recommended to 69% of patients; however, post-testing, a change in the RT recommendation was made for 42% of patients compared with the pre-testing recommendation; the percentage of women who were recommended RT decreased by 20%. For women initially recommended not to receive an RT pre-test, 35% had their recommendation changed to add RT following testing, while post-test, 46% of patients had their recommendation changed to omit RT after an initial recommendation for RT. When considered in conjunction with other clinicopathologic factors, the elevated DCISionRT score risk group (DS > 3) had the strongest association with an RT recommendation (odds ratio 43.4) compared with age, grade, size, margin status, and other factors.
Conclusions
DCISionRT provided information that significantly changed the recommendations to add or omit RT. Compared with traditional clinicopathologic features used to determine recommendations for or against RT, the factor most strongly associated with RT recommendations was the DCISionRT result, with other factors of importance being patient preference, tumor size, and grade.
Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Long-term outcomes of invasive ipsilateral breast tumor recurrences after lumpectomy in NSABP B-17 and B-24 randomized clinical trials for DCIS.
- Record: found
- Abstract: found
- Article: not found
Overview of the randomized trials of radiotherapy in ductal carcinoma in situ of the breast.

- Record: found
- Abstract: found
- Article: found