- Record: found
- Abstract: found
- Article: found
Probiotics in Inflammatory Bowel Diseases and Associated Conditions
Read this article at
Abstract
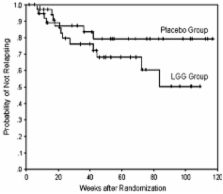
A complex set of interactions between the human genes encoding innate protective functions and immune defenses and the environment of the intestinal mucosa with its microbiota is currently considered key to the pathogenesis of the chronic inflammatory bowel diseases (IBD). Probiotics offer a method to potentially alter the intestinal microbiome exogenously or may provide an option to deliver microbial metabolic products to alter the chronicity of intestinal mucosal inflammation characterizing IBD. At present, there is little evidence for the benefit of currently used probiotic microbes in Crohn’s disease or associated conditions affecting extra-intestinal organs. However, clinical practice guidelines are now including a probiotic as an option for recurrent and relapsing antibiotic sensitive pouchitis and the use of probiotics in mild ulcerative colitis is provocative and suggests potential for benefit in select patients but concerns remain about proof from trials.
Related collections
Most cited references69
- Record: found
- Abstract: found
- Article: not found
Genome-wide association identifies multiple ulcerative colitis susceptibility loci.
- Record: found
- Abstract: found
- Article: not found
Smoking and inflammatory bowel disease: a meta-analysis.
- Record: found
- Abstract: found
- Article: not found