- Record: found
- Abstract: found
- Article: found
Neuroinflammation and subarachnoid hemorrhage: a revised look at the literature
Read this article at
Abstract
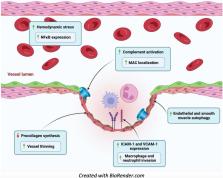
A key topic for aneurysmal subarachnoid hemorrhage is neuroinflammation. Neuroinflammation can predispose to aneurysm formation and rupture. Neuroinflammation can also result from the blood breakdown products after aneurysm rupture. Recent evidence has shown that perpetual neuroinflammation can contribute to vasospasm and hydrocephalus. Targeting neuroinflammation is a novel mechanism for preventing subsequent neurologic sequalae. In this review, we highlight the pathophysiology of aneurysm formation, the neuroinflammatory surge after rupture including the involved cytokines, and ultimately tie in the contributory clinical relevance. In the last sections, we look at the pre-clinical data and novel avenues for further discovery. This paper will be a useful resource to both the clinician and scientific investigator.
Related collections
Most cited references132
- Record: found
- Abstract: found
- Article: not found
Structural and functional features of central nervous system lymphatics

- Record: found
- Abstract: found
- Article: found
Macrophage Polarization: Different Gene Signatures in M1(LPS+) vs. Classically and M2(LPS–) vs. Alternatively Activated Macrophages
- Record: found
- Abstract: found
- Article: not found