- Record: found
- Abstract: found
- Article: found
Dual vs. mono antiplatelet therapy for acute ischemic stroke or transient ischemic attack with evidence of large artery atherosclerosis
Read this article at
Abstract
Background and purpose
Current pieces of evidence support the short-term use of dual antiplatelet (DAPT) in minor ischemic stroke or transient ischemic attack (TIA) based on the studies performed in patients with a broad range of non-cardioembolic stroke mechanisms. However, the efficacy and safety of DAPT use in ischemic stroke patients with large artery atherosclerosis (LAA) are still uncertain. We undertook a systemic search and formal meta-analysis to compare DAPT vs. mono-antiplatelet therapy (MAPT) in patients with etiology specifically presumed to be symptomatic LAA.
Methods
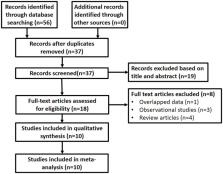
We conducted a systemic online search for completed randomized controlled trials that (1) compared DAPT vs. MAPT in patients with acute ischemic stroke or TIA, and (2) were confined to or had available subgroup data regarding population with symptomatic extra- or intracranial artery stenosis. Study-level meta-analysis was performed for outcomes, including ischemic stroke (IS) recurrence, intracranial hemorrhage (ICH), and major bleeding with the Mantel-Haenszel method and random effect models, and was described as risk difference (RD) and 95% CI.
Results
A total of 10 trials including 5,004 patients were pooled. Comparing to MAPT, DAPT significantly reduced IS recurrence (5.99 vs. 9.55%, RD: −3%, 95% CI: −5 –0%). Across all agents, out of 100 treated patients, 3 fewer had a recurrent ischemic stroke with DAPT. The safety endpoints including ICH (0.28 vs. 0.32%, RD: 0%, 95% CI: −0 –0%) and major bleeding (0.73 vs. 0.51%, RD: 0%, 95% CI: −0 –0%) did not differ significantly.
Related collections
Most cited references27
- Record: found
- Abstract: found
- Article: not found
Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement
- Record: found
- Abstract: not found
- Article: not found
Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment
- Record: found
- Abstract: found
- Article: not found