- Record: found
- Abstract: found
- Article: found
Detection of Migrainous Infarction with Formal Visual Field Testing: A Case Report
Read this article at
Abstract
Introduction
Cerebrovascular accidents (CVA) of the posterior circulation are a rare complication of migraine, and present with atypical CVA symptomatology.
Case Report
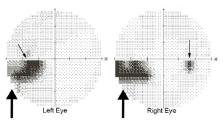
A 49-year-old-male presented with complaint of persistent visual aura and resolved mild cephalgia. His exam corroborated his reported incomplete left inferior quadrantanopia, and was confirmed by immediate formal optometry evaluation. Occipital CVA was confirmed on admission.
Conclusion
Migrainous strokes of posterior circulation should be considered as a potential diagnosis in any headache patient with persistent visual aura. This case suggests that incorporation of formal visual field testing in the emergent setting can shorten the time required for diagnosis in certain circumstances.
Related collections
Most cited references10
- Record: found
- Abstract: found
- Article: not found
Homonymous hemianopia in stroke.
- Record: found
- Abstract: found
- Article: not found
Homonymous visual field defects and stroke in an older population.
- Record: found
- Abstract: found
- Article: not found
