- Record: found
- Abstract: found
- Article: found
Management of acetabular bone loss in revision total hip replacement: a narrative literature review

Read this article at
Abstract
Background and Objective
Due to growing numbers of primary total hip replacement (THR), the revision THR burden is also increasing. Common indications for revision are osteolysis, infection, instability, and mechanical failure of implants, which can cause acetabular bone loss. Massive acetabular bone defects and pelvic discontinuity are extremely challenging problems. Many techniques have been utilized to address bone loss while maintaining a stable revision THR. Structural allografts, cemented prosthesis, reconstruction cages, and custom triflanged implants have all been used successfully albeit with relatively high complications rates. We have tried to highlight emerging trends to utilize Custom Made Monoflange or Triflange Acetabular Components to reconstruct massive acetabular defects with favourable midterm implant survival, better functional outcomes, relatively lesser complications, and almost similar cost of prosthesis as compared to conventional reconstruction techniques. However, long-term data and study is still recommended to draw a definitive conclusion.
Methods
In this narrative review article, we searched PubMed and Cochrane for studies on managing acetabular bone loss in revision THR with a focus on recent literature for mid to long-term outcomes and compared results from various studies on different reconstruction methods.
Key Content and Findings
Hemispherical cementless acetabular prosthesis with supplemental screws are commonly utilized to manage mild to moderate acetabular bone loss. Recent trends have shown much interest and paradigm shift in patient specific custom triflange acetabular components (CTAC) for reconstructing massive acetabular defects and pelvic discontinuity. Studies have reported high patient satisfaction, improved patient reported daily functioning, high mid-term implant survival, similar complications, and encouraging all cause re-revision rate. However, more prospective and quality studies with larger sample sizes are needed to validate the superiority of CTACs over conventional acetabular implants.
Conclusions
There is no consensus regarding the best option for reconstructing massive acetabular defects. Thorough preoperative workup and planning is an absolute requirement for successful revision THR. While most of the moderate acetabular bone loss can be managed with cementless hemispherical acetabular shells with excellent long-term outcomes, reconstructing massive acetabular bone defects in revision THR remains a challenge. Depending on the size and location of the defect, various constucts have demonstrated long-term success as discussed in this review, but complications are not negligible. CTACs provide a treatment for massive bone loss that may be otherwise difficult to achieve anatomic stability with other constructs. Although long-term data is sparse, the cost and complication rate is comparable to other reconstruction methods.
Related collections
Most cited references44
- Record: found
- Abstract: not found
- Article: not found
The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria
- Record: found
- Abstract: found
- Article: found
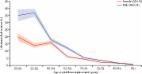
The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study
- Record: found
- Abstract: found
- Article: not found