- Record: found
- Abstract: found
- Article: found
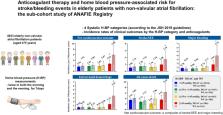
Anticoagulant therapy and home blood pressure-associated risk for stroke/bleeding events in elderly patients with non-valvular atrial fibrillation: the sub-cohort study of ANAFIE registry
Read this article at
Abstract
The benefits of direct oral anticoagulants (DOACs) and warfarin in elderly Japanese patients with non-valvular atrial fibrillation (NVAF) and high home systolic blood pressure (H-SBP) are unclear. This sub-cohort study of the ANAFIE Registry estimated the incidence of clinical outcomes in patients receiving anticoagulant therapy (warfarin and DOACs) stratified by H-SBP levels (<125 mmHg, ≥125–<135 mmHg, ≥135–<145 mmHg and ≥145 mmHg). Of the overall ANAFIE population, 4933 patients who underwent home blood pressure (H-BP) measurements were analyzed; 93% received OACs (DOACs: 3494, 70.8%; warfarin: 1092, 22.1%). In the warfarin group, at <125 mmHg and ≥145 mmHg, the respective incidence rates (per 100 person-years) were 1.91 and 5.89 for net cardiovascular outcome (a composite of stroke/systemic embolic events (SEE) and major bleeding), 1.31 and 3.39 for stroke/SEE, 0.59 and 3.91 for major bleeding, 0.59 and 3.43 for intracranial hemorrhage (ICH), and 4.01 and 6.24 for all-cause death. Corresponding incidence rates in the DOACs group were 1.64 and 2.65, 1.00 and 1.88, 0.78 and 1.69, 0.55 and 1.31, and 3.43 and 3.51. In warfarin-treated patients, the incidence rates of net cardiovascular outcome, stroke/SEE, major bleeding, and ICH were significantly increased at H-SBP ≥ 145 mmHg versus <125 mmHg. In the DOAC group, although there was no significant difference between H-SBP < 125 mmHg and ≥145 mmHg, the incidence rates of these events tended to increase at ≥145 mmHg. These results suggest that strict BP control guided by H-BP is required in elderly NVAF patients receiving anticoagulant therapy.

Related collections
Most cited references15
- Record: found
- Abstract: found
- Article: not found
Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients.
- Record: found
- Abstract: not found
- Article: not found
The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2019)
- Record: found
- Abstract: found
- Article: not found