- Record: found
- Abstract: found
- Article: not found
Restless legs syndrome secondary to pontine infarction: Clinical analysis of five cases
Read this article at
Abstract
Objective
Pontine infarction is a common type of stroke in the cerebral deep structures, resulting from occlusion of small penetrating arteries, may manifest as hemi-paralysis, hemi-sensory deficit, ataxia, vertigo, and bulbar dysfunction, but patients presenting with restless legs syndrome (RLS) are extremely rare. Herein, we reported five cases with RLS as a major manifestation of pontine infarction.
Methods
Five cases of pontine infarction related RLS were collected from July 2013 to February 2016. The diagnosis of RLS was made according to criteria established by the International RLS Study Group (IRLSSG) in 2003. Neurological functions were assessed according to the National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS). Severity of RLS was based on the International RLS Rating Scale (IRLS-RS). Sleep quality was assessed by Epworth Rating Scale (ERS), and individual emotional and psychological states were assessed by Hamilton Depression Scale (HDS) and Hamilton Anxiety Scale (HAS).
Results
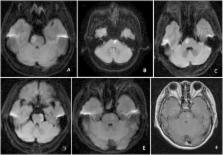
The laboratory data at the onset including hemoglobin, serum concentration of homocysteine, blood urea nitrogen (BUN), creatinine, electrolytes, and thyroid hormones were normal. The electroencephalogram (EEG), lower-extremity somatosensory evoked potential (SEP), and nerve conduction velocity (NCV) in four limbs were normal. The average period of follow-up was 34.60 ± 12.76 months. The MRI examination showed acute or subacute pontine infarction lesions, 3 cases in the rostral inner side, 1 case in the rostral lateral and inner side, and 1 case in rostral lateral side. The neurological deficits included weakness in 4 cases, contralateral sensory deficit in 1 case, and ataxia in 2 cases. All 5 patients presented with symptom of RLS at or soon after the onset of infarction and 4 patients experienced uncomfortable sensations in the paralyzed limbs contralateral to the ischemic lesion. Their neurological deficits improved significantly 2 weeks later, but the symptoms of RLS did not resolve. Among them, 3/5 patients were treated with dopaminergic drugs. At the end of the follow-up, RLS symptom eventually resolved in 3 patients but persisted in two. The IRLS-RS, NIHSS and mRS scores were significantly lower at the onset than those at the last follow-up ( P = 0.035, 0.024 and 0.049, respectively). However, there was no significant difference in the ERS, HDS and HAS scores ( P = 0.477, 0.226 and 0.778, respectively).
Related collections
Most cited references11
- Record: found
- Abstract: found
- Article: not found
Restless legs syndrome: diagnostic criteria, special considerations, and epidemiology. A report from the restless legs syndrome diagnosis and epidemiology workshop at the National Institutes of Health.
- Record: found
- Abstract: found
- Article: not found
Poststroke restless legs syndrome and lesion location: anatomical considerations.
- Record: found
- Abstract: found
- Article: not found
