- Record: found
- Abstract: found
- Article: found
Time to peak bilirubin concentration and advanced AKI were associated with increased mortality in rheumatic heart valve replacement surgery patients with severe postoperative hyperbilirubinemia: a retrospective cohort study
Read this article at
Abstract
Background
Hyperbilirubinemia after heart valve surgery (HVS) with cardiopulmonary bypass is frequently observed and associated with worse outcomes. We investigated the characteristics and prognosis of patients with severe hyperbilirubinemia after HVS for rheumatic heart disease (RHD) to identify the clinical outcomes and potential risk factors.
Methods
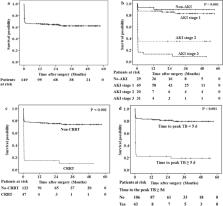
Between 2015 and 2018, patients who underwent HVS in the cardiac surgery intensive care unit of our hospital were retrospectively screened. Risk factors for acute kidney injury (AKI), the requirement for continuous renal replacement therapy (CRRT), and in-hospital and long-term mortality were identified by univariate and multivariate analyses. The patient survival proportion was graphically presented with the Kaplan–Meier method.
Results
A total of 149 patients who underwent HVS for RHD and had severe postoperative hyperbilirubinemia were included. Of the included patients, 80.5% developed postoperative AKI, and 18.1% required CRRT. The in-hospital mortality was 30.2%. Backward logistic regression analysis showed that the time to peak TB concentration (odds ratio [OR] 1.557, 95% confidence interval [CI] 1.259–1.926; P < 0.001) and advanced AKI (stage 2 and 3 AKI) (OR 19.408, 95% CI 6.553–57.482; P < 0.001) were independent predictors for in-hospital mortality. The cutoff value of the time to peak TB levels for predicting in-hospital mortality was 5 postoperative days.
Related collections
Most cited references43

- Record: found
- Abstract: found
- Article: found
Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1)
- Record: found
- Abstract: found
- Article: not found
Cardiac surgery-associated acute kidney injury: risk factors, pathophysiology and treatment
- Record: found
- Abstract: found
- Article: not found