- Record: found
- Abstract: found
- Article: found
Assessment of a Non Invasive Brain Oximeter in Volunteers Undergoing Acute Hypoxia
Read this article at
Abstract
Introduction
Research in traumatic brain injury suggests better patient outcomes when invasive oxygen monitoring is used to detect and correct episodes of brain hypoxia. Invasive brain oxygen monitoring is, however, not routinely used due to the risks, costs and technical challengers. We are developing a non-invasive brain oximeter to address these limitations. The monitor uses the principles of pulse oximetry to record a brain photoplethysmographic waveform and oxygen saturations. We undertook a study in volunteers to assess the new monitor.
Patients and Methods
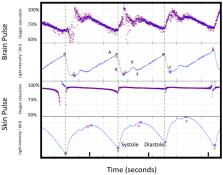
We compared the temporal changes in the brain and skin oxygen saturations in six volunteers undergoing progressive hypoxia to reach arterial saturations of 70%. This approach provides a method to discriminate potential contamination of the brain signal by skin oxygen levels, as the responses in brain and skin oxygen saturations are distinct due to the auto-regulation of cerebral blood flow to compensate for hypoxia. Conventional pulse oximetry was used to assess skin oxygen levels. Blood was also collected from the internal jugular vein and correlated with the brain oximeter oxygen levels.
Results
At baseline, a photoplethysmographic waveform consistent with that expected from the brain was obtained in five subjects. The signal was adequate to assess oxygen saturations in three subjects. During hypoxia, the brain's oximeter oxygen saturation fell to 74%, while skin saturation fell to 50% (P<0.0001). The brain photoplethysmographic waveform developed a high-frequency oscillation of ~7 Hz, which was not present in the skin during hypoxia. A weak correlation between the brain oximeter and proximal internal jugular vein oxygen levels was demonstrated, R 2=0.24, P=0.01.
Related collections
Most cited references45

- Record: found
- Abstract: found
- Article: found
The pulsating brain: A review of experimental and clinical studies of intracranial pulsatility
- Record: found
- Abstract: found
- Article: not found
Brain Oxygen Optimization in Severe Traumatic Brain Injury Phase-II
- Record: found
- Abstract: found
- Article: not found