- Record: found
- Abstract: found
- Article: found
SUPPORT Tools for evidence-informed health Policymaking (STP) 17: Dealing with insufficient research evidence
Read this article at
Abstract
This article is part of a series written for people responsible for making decisions about health policies and programmes and for those who support these decision makers .
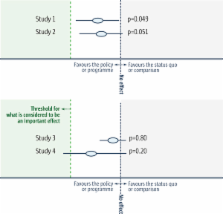
In this article, we address the issue of decision making in situations in which there is insufficient evidence at hand. Policymakers often have insufficient evidence to know with certainty what the impacts of a health policy or programme option will be, but they must still make decisions. We suggest four questions that can be considered when there may be insufficient evidence to be confident about the impacts of implementing an option. These are: 1. Is there a systematic review of the impacts of the option? 2. Has inconclusive evidence been misinterpreted as evidence of no effect? 3. Is it possible to be confident about a decision despite a lack of evidence? 4. Is the option potentially harmful, ineffective or not worth the cost?
Related collections
Most cited references27

- Record: found
- Abstract: found
- Article: found
SUPPORT Tools for evidence-informed health Policymaking (STP) 1: What is evidence-informed policymaking?
- Record: found
- Abstract: found
- Article: not found
Effects of policy options for human resources for health: an analysis of systematic reviews.

- Record: found
- Abstract: found
- Article: found