- Record: found
- Abstract: found
- Article: found
Does the World Need Plant Medicines?
editorial
Read this article at
There is no author summary for this article yet. Authors can add summaries to their articles on ScienceOpen to make them more accessible to a non-specialist audience.
Abstract
Our species has always used plants as medicines, during our 200,000 year existence.
This is made obvious by the plant medicines found in mummy burials, around the world,
dating back thousands of years. Human beings evolved using plant medicines to stay
alive. This has resulted in a genetic selection in which those who were healed by
plant medicines and survived were able to pass on their genes. Modern humans must
continue to use plant medicines.
When a Traditional Healer is asked how her people learned how to use a specific plant
medicine, the answer is usually that God taught them. Each of us has a spiritual sense
that can be used to seek answers [1]. Finding a new plant medicine involves fasting,
praying, and spending as much as four days with the plant that will become a new medicine
[2]. Traditional Healers are still the major or only source of healthcare for many
regions of the world. The loss of Traditional Healers in some areas has resulted in
major changes in healthcare, sometimes to the detriment of the people [3,4]. Since
Traditional Healers may be religious leaders also, they provide moral direction for
the community. The displacement of traditional religious beliefs has been detrimental
in some regions.
The most powerful medicine each person has is the human body. The body heals itself.
When the body is in balance, it can heal itself of many conditions, in other words,
it can prevent many diseases [5,6]. Patients should be taught what balance is and
how to maintain balance, including staying thin and strong.
Drugs are not magic bullets that cure diseases. They help the body heal itself. Even
antibiotics and anticancer drugs are of no use when the immune and defense systems
are not functioning well. In many clinical trials, the placebo works as well as the
drug because of the body’s ability to heal itself [7].
Clinical trials are useful to demonstrate what a plant medicine can be used to treat
and to demonstrate safety. Useful information can be derived from placebo controlled
clinical trials, from clinical trials that compare a new medicine to an old medicine
and from other clinical trial designs. Many different clinical trial designs are appropriate.
The double blind, randomized, placebo controlled clinical trial should not be used
as the gold standard of clinical trial design [7]. Many other designs are just as
valid and may be less risky to patients, such as patients who are put on the placebo.
Clinical trials are frequently abused. Drugs are shown to help with one disease symptom
and are approved for use, even though they are very toxic. Many of the oral medicines
used to treat pain are dangerous drugs that kill many patients. Oral opioids kill
about 67,000 people in the USA every year. Oral nonsteroidal anti-inflammatory drugs
have been estimated to kill at least 50,000 USA patients every year from ulcers, heart
attacks, and strokes [8,9]. The most dangerous way to treat pain is with oral or injected
pain medications. Some of the drugs approved for type 2 diabetes cause heart disease.
Some of the drugs approved for heart disease cause type 2 diabetes. Just because a
drug is useful for one symptom, does not mean the drug should be used.
Drugs are frequently used as if they were the only possible treatment for a disease.
Patients seem to have become convinced that drugs can take care of any disease. Prevention
is the best treatment for many chronic diseases that plague the modern world. Type
2 diabetes, heart disease, and osteoarthritis are caused by excess visceral fat, obesity
[10,11]. Visceral fat secretes toxic lipids and akipokines that cause these diseases.
Toxic adipokines also potentiate the formation of cancer in the body [10]. As modern
man has become more sedentary and obese, these diseases have increased greatly, much
to the benefit of the pharmaceutical industry. A better option is to live in balance
and prevent diseases.
In the midst of our crisis of drug over use and abuse, patients must find alternative
choices for healthcare. Prevention should always be the healthcare of choice. When
medicines are needed, many plant medicines continue to be available in most of the
world. In the United States, medicines are tightly regulated by the Food and Drug
Administration. Due to this strict regulation, few indigenous American plant medicines
are readily available. Patients must find Traditional Healers who still know how to
make Native American plant medicines [2]. Plant medicines made from European plants
are much more available in the United States.
In the current publication, Edenta, Okoduwa, and Okpe teach about the use of plant
medicines in Nigeria [12]. Musa acuminata is a species of banana that originally comes
from Southeast Asia and has been cultivated for over 8000 years. It was probably introduced
into Nigeria long ago. Traditional Healers in Nigeria use M. acuminata peels in the
treatment of their patients. There are several cultivars of M. acuminata, each with
different pharmacology and toxicology. The work of Edenta and coworkers demonstrates
that some plant medicines may not be safe for human use.
Kinda et al. discuss the use of plant medicines to treat neuropsychiatric conditions
by Traditional Healers in Burkina Faso [13]. Neuropsychiatric conditions existed during
ancient times and were a burden for the community. In traditional villages, each member
of the village has a job that is critical to the survival of the village. If a neuropsychiatric
condition prevented a village member from being productive, the Traditional Healer
had to find a way to help. In Burkina Faso, Traditional Healers use 66 different plant
species to make medicines for neuropsychiatric conditions. Modern medicine relies
on the use of dopamine 2 receptor antagonists to treat psychosis. These drugs cause
extrapyramidal side effects in 50% of patients, weight gain in most patients, and
potentially irreversible tardive dyskinesia in 68% of patients treated for 25 years.
Even though dopamine 2 receptor antagonists are useful in neuropsychiatric conditions,
their toxicity is a concern. Modern medicine may be wise to learn from the Traditional
Healers of Burkina Faso.
Tchuenmogne et al. describe their work to find biologically-active compounds from
Terminalia mantaly, the Madagascar almond [14]. They describe several compounds that
are interesting antifungal agents. Pathak, Upreti, and Dikshit provide evidence of
antifungal compounds from a lichen, Usnea orientalis [15]. The treatment of fungal
infections has become very important and difficult due to the huge increase in type
2 diabetes in the world. Diabetics are very susceptible to fungal infections.
Balogun et al. examine an endangered medicinal plant, Oncoba spinosa. This small tree
grows in many areas of Africa [16]. The fruit is used in Traditional Healing in Nigeria.
Although several reports have examined the Phytochemistry of the plant, Balogun and
coworkers found a compound not previously seen in the leaves. The compound, flacourtin,
is also found in an Indian plant that is used in Traditional Healing.
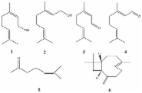
Al-Tamimi, Rastall, and Abu-Reidah report on the antioxidant and toxic properties
of nine essential oils [17]. In order to produce an essential oil, a large amount
of plant material is heated, such as in a steam bath, until the volatile compounds
from the plant distill. Essential oils have been used in European Traditional Healing.
Some essential oils are very toxic, even to the skin. El-Tamimi and coworkers found
that ginger, chamomile, and African rue essential oils were of interest. They also
found that some essential oils are not pharmacologically potent and suggest that storage
and preparation conditions may be important with these products.
Ouedraogo and Kiendregeogo discuss the antibiotic potency of Anogeissus leiocarpus,
African birch [18]. The plant is used by Traditional Healers in wound healing. Methanol
extracts of the plant were examined against bacterial strains. This work shows the
importance of wound healing in traditional villages. There are probably several alternative
treatments that modern medicine should consider for the treatment of difficult wounds,
such as diabetic skin ulcers.
Santos et al. present evidence of cytotoxic and antimicrobial compounds in an essential
oil from Lippia alba, bushy mattgrass, which comes from the Caribbean, Central and
South America [19]. They found 39 compounds, of which many are monoterpenes. Some
monoterpenes from bushy mattgrass may be useful against fungal infections.
Khurm et al. provide evidence of the safety of Heliotropium strigosum, called Kharsan,
Gorakh pam, and Bhangra in Pakistan [20]. The plant is used in Traditional healing
for respiratory and GI problems. Plant preparations have low toxicity against several
bacteria and fungi. The medicine is known to contain compounds that relax inflamed
lung tissue.
Work from my laboratory, by Wang et al., provides controversial evidence for the use
of a plant medicine in the treatment of Alzheimer’s disease [21]. In ancient times,
some older people suffered from what is now called Alzheimer’s disease. Chumash Healers
found that the berries of Heteromeles arbutifolia, toyon, a California plant, helped
slow down the progression of the disease. White people labeled the plant poisonous,
due to their racist beliefs that plants used by Indians must be poisonous. The plant
has not been carefully examined until now. My group found several interesting compounds
in the plant and demonstrated the safety of the berries in several patients. All of
the clinical trials of new Alzheimer’s disease drugs have failed [22]. Perhaps this
plant medicine should be examined in clinical trials.
Olorunnisola, Fadahunsi, and Adegbola teach us about Traditional Healing with Sphenocentrum
jollyanum, aduro kokoo. The plant is used as a medicine in several West African countries
[23]. Alkaloids, saponins, flavonoids, and other compounds are found in the plant.
Traditional Healers have found several uses for the plant in treating their patients,
including high blood pressure. Black Americans are resistant to several antihypertensive
drugs. It may be wise to use this plant in resistant patients.
Rodriguez Villanueva, Esteban, and Rodriguez Villanueva discuss the use of Marrubium
vulgare, horehound in type 2 diabetes [24]. The authors find that clinical trials
performed with the plant were flawed. They suggest finding better clinical trial methods
in order to accurately assess the value of the plant. This is a constant problem in
plant medicine clinical trials. In the USA, the Food and Drug Administration and the
National Center for Complementary and Integrative Health insist on using hydro-alcoholic
extracts of American plants or similar preparations in clinical trials, even though
Traditional Healers have never used these preparations. The purpose of these clinical
trials, therefore, is to disprove the efficacy of the plant medicines. This is a vivid
reminder of the anti-Indian racism that permeates these federal agencies.
Teng et al. provide a case report of a woman who had a successful pregnancy after
being treated with Chinese herbal medicines. In vitro fertilization had failed in
the woman [25]. This case reinforces the power of herbal medicines.
The purpose of the current writing is to educate the healthcare community about the
importance of plant medicines. Plant medicines can be safe and efficacious even when
modern drugs fail. Plant medicines should be used in the traditional preparations
and by the traditional routes. One of the advantages of plant medicines is that they
contain several active compounds that all add to therapy. They may even potentiate
or synergize the effects of other compounds in the medicine. The author of the current
writing encourage the modern use of plant medicines after performing realistic clinical
trials.
Related collections
Most cited references21

- Record: found
- Abstract: found
- Article: found
Chemical Composition, Cytotoxic, Apoptotic and Antioxidant Activities of Main Commercial Essential Oils in Palestine: A Comparative Study

- Record: found
- Abstract: found
- Article: found
Medicinal Plants Used for Neuropsychiatric Disorders Treatment in the Hauts Bassins Region of Burkina Faso
Prosper T. Kinda, Patrice Zerbo, Samson Guenne … (2017)
- Record: found
- Abstract: found
- Article: found
Cytotoxic and Antimicrobial Constituents from the Essential Oil of Lippia alba (Verbenaceae)
Nara dos Santos, Renata Pascon, Marcelo A. Vallim … (2016)