- Record: found
- Abstract: found
- Article: found
Effectiveness and safety of a robot-assisted 3D personalized template in 125I seed brachytherapy of thoracoabdominal tumors
Read this article at
Abstract
Purpose
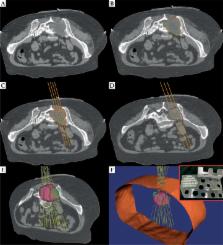
This research aims to evaluate the effectiveness and safety of a robot-assisted 3D personalized template in 125I seed brachytherapy of thoracoabdominal tumors.
Material and methods
Forty-three patients with different tumors were involved in this research between 2013 and 2015. They were all eligible to 125I seed implantation based on robot-assisted 3D personalized template. Meanwhile, 51 patients with similar tumors, which were treated with a conventional coplanar template, were involved for comparison. Follow-up was carried out after the surgery to evaluate the therapeutic efficacy, including overall survival (OS) of the patient and local control (LC) of the tumor. Complications were also summarized to evaluate the safety. Besides, statistical analysis was achieved to investigate possible factors associated with the result.
Results
In the robot-assisted 3D personalized template-guided brachytherapy, the median target volume treated by the prescription dose (V 100) was 95.3% (range, 92.4-109.8), and the median dose administered to 90% of the target volume (D 90) was 126.1 Gy (range, 114.2-132.0), improved 5% and 8% compared with the conventional template-guided brachytherapy, respectively. The median OS was 30 months (95% CI: 19.4-40.6) and the rates of 2-year OS and LC were 58.1% and 86.0%, respectively. The median OS was prolonged 10 months and the 2-year OS and LC were improved 18.9% and 23.3% compared with the conventional template-guided brachytherapy, respectively.
Related collections
Most cited references26
- Record: found
- Abstract: found
- Article: not found
Impact of Radiotherapy on Complications and Patient-Reported Outcomes After Breast Reconstruction
- Record: found
- Abstract: found
- Article: not found
Prognostic factors following curative resection for pancreatic adenocarcinoma: a population-based, linked database analysis of 396 patients.
- Record: found
- Abstract: found
- Article: not found
