- Record: found
- Abstract: found
- Article: found
Regional Requirements Influence Adoption of Exertional Heat Illness Preparedness Strategies in United States High Schools
Read this article at
Abstract
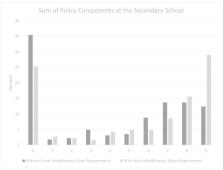
Background and objectives: Exertional heat stroke (EHS) continues to be a prevalent health issue affecting all athletes, including our pediatric populations. The purpose of this study was to evaluate the effect of a state policy requirement for EHS prevention and treatment on local high school policy adoption in the United States (US). Materials and Methods: Athletic trainers (ATs) from high schools across the US participated in an online survey ( n = 365). This survey inquired about their compliance with nine components of an EHS policy which was then compared to their state requirements for the policies. Evaluation of the number of components adopted between states with a requirement versus states without a requirement was conducted with a Wilcoxon Sign Rank test. Finally, an ordinal logistic regression with proportional odds ratios (OR) with 95% confidence intervals (CI) were run to determine the effect of a state requirement and regional differences on the number of components adopted. Results: ATs working in states with a requirement reported adoption of more components in their heat modification policy compared to states that did not require schools to develop a heat modification policy (with requirement mean = 5.34 ± 3.68, median = 7.0; without requirement mean = 4.23 ± 3.59, median = 5.0; Z = −14.88, p < 0.001). ATs working in region 3 (e.g., hotter regions) reported adopting more components than those in region 1 (e.g., cooler regions) (OR = 2.25, 95% CI: 1.215–4.201, p = 0.010). Conclusions: Our results demonstrate a positive association between state policy requirements and subsequently increased local policy adoption for EHS policies. Additionally, the results demonstrate that regional differences exist, calling for the need for reducing disparities across the US. These findings may imply that policy adoption is a multifactorial process; furthermore, additional regional specific investigations must be conducted to determine the true determinants of high school policy adoption rates for EHS policies.
Related collections
Most cited references30
- Record: found
- Abstract: found
- Article: not found
American College of Sports Medicine position stand. Exertional heat illness during training and competition.
- Record: found
- Abstract: found
- Article: not found
National Athletic Trainers' Association Position Statement: Exertional Heat Illnesses.
- Record: found
- Abstract: found
- Article: not found