- Record: found
- Abstract: found
- Article: found
Meningeal “Lazarus Response” to Lorlatinib in a ROS1-Positive NSCLC Patient Progressing to Entrectinib

Read this article at
Abstract
Background
ROS1 tyrosine kinase inhibitors (TKIs) have showed activity and efficacy in ROS1-rearranged non-small cell lung cancer (NSCLC). In the clinical practice, besides the utilization of crizotinib, less is known about the best treatment strategies involving additional, new-generation TKIs for the sequential treatment of ROS1-positive NSCLC patients.
Case Presentation
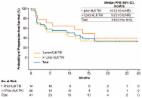
A patient suffering from a ROS1-rearranged lung adenocarcinoma, after receiving cisplatin-pemetrexed chemotherapy, was treated with entrectinib, a new-generation ALK/ROS1/NTRK inhibitor. After 16 months, central nervous system (CNS) metastases appeared, without extra-cerebral disease progression. Stereotactic brain radiotherapy was performed and entrectinib was maintained, due to the global systemic disease control. Approximately one month after radiotherapy, thoracic and meningeal progressions were detected, the latter highly symptomatic with neurocognitive disorders, visual hallucinations and worsening of psycho-motor impairment. A lumbar puncture was positive for tumor cells and for an EZR-ROS1 fusion. The administration of lorlatinib (a third-generation ALK/ROS1 inhibitor) prompted an extremely rapid improvement of clinical conditions, anticipating the positive results observed at radiologic evaluation that confirmed the disease response still ongoing after nine months since treatment start.
Discussion
With the expanding availability of targeted agents with differential activity on resistance mechanism and on CNS disease, choosing wisely the best treatment strategies is pivotal to assure the best clinical outcomes in oncogene-addicted NSCLC patients. Here we have reported lorlatinib reverted an almost fatal meningeal carcinomatosis developing during entrectinib in a ROS1-positive NSCLC patient.
Related collections
Most cited references27
- Record: found
- Abstract: not found
- Article: not found
Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up†
- Record: found
- Abstract: found
- Article: found
Lorlatinib in ALK - or ROS1 -rearranged non-small cell lung cancer: an international, multicenter, open-label phase 1 trial
- Record: found
- Abstract: found
- Article: found